Background: Effective communication and care coordination between inpatient and outpatient teams are essential for safe care transitions. Currently there is infrequent communication between PCPs and Hospitalists around the time of discharge. Often, the PCPs are not aware of pending tests that need follow-up, and in the cases where they are aware of a pending test, it is unclear who is responsible for follow-up (due to ambiguity of who will perform the follow up within the discharge summary documentation.) Prior work has found that as many as 41% of patients discharged from a medicine service have a test pending at the time of discharge. We know that poor communication of tests pending and lack of responsibility for follow up has been attributed to medical errors or delay in care. The objective of this study was to determine the current communication practices between PCPs and Hospitalists with regard to tests pending at the time of patient discharge from the inpatient medicine service.
Purpose: Our aim was to increase the percentage of discharge summaries with a clear follow-up plan for the tests pending at the time of discharge documented in the discharge summary from the current baseline of 13% to 50% across general medicine patients discharged from the Hospitalist service on two of the inpatient medical services (Three floors: Ellison 12, Phillips 20 and Ellison 19. )
Description: Methods: We administered a cross sectional web-based survey to all PCPs (n=165) who admit patients to the hospitalist/inpatient medical team and all hospitalists (n=96) working at a large academic hospital, Massachusetts General Hospital. The goal of the survey was to explore communication between PCPs and hospitalists around the time of discharge. We used descriptive statistics to compare communication practices between PCPs and hospitalists.
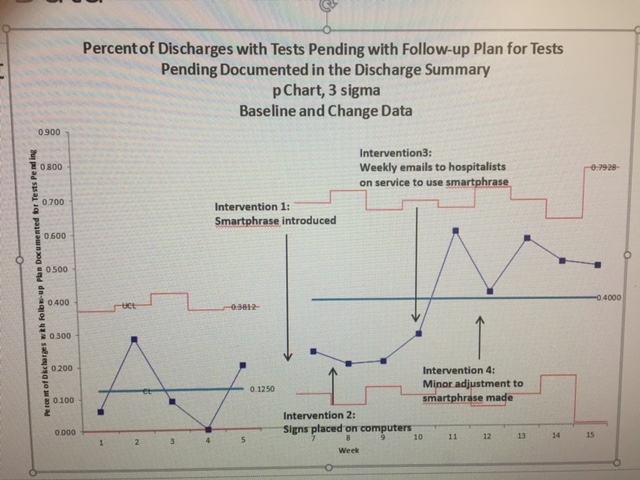
After analysis of the survey results, we met with a team of PCPs and Hospitalists to brainstorm the need and plan for documentation, a plan for intervention was put into place. The interventions were initially done by utilizing the EMR by creating and pushing the smartphrase to the Hospital Medicine Unit within EPIC. The hospital medicine group was educated about the need for and how to use the smartphrase to insure documentation. To improve compliance, the Inpatient Administrative coordinators were asked to include a reminder in their daily email to group. Signs were subsequently posted on the computers to remind providers to use the smartphrase in their daily work. Finally, weekly emails were sent to all providers that would be on service that week to remind them to use the smartphrase to document pending studies. Toward the end of the assessment period and beyond, adjustments were made to the smartphrase as well as service wide ongoing education sessions.
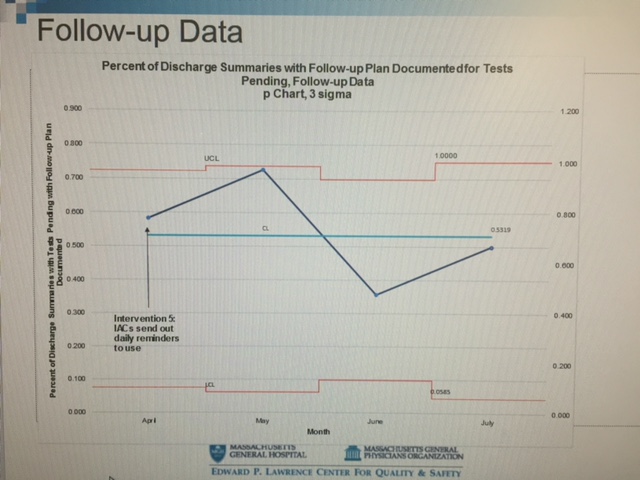
Conclusions: Following implementation of Epic Smartphrase and multiple education strategies there was improvement in the documentation of follow-up plans for tests pending within discharge summaries. Overall the outcome measure–the rate of documentation of a follow-up plan in the discharge summary– increased from an average of 13% to 40% on 2 of the hospitalist services (3 floors). Feedback from PCPs indicates recognition of improved documentation.
Behavior change is difficult. Increasing streamlined reminders down the road would be helpful to increase use of smartphrase and long term adoption of improved documentation.