Background: VTE (Venous Thromboembolism) is the most common preventable cause of hospital-related deaths and claim more than 100,000 lives a year in the United States. Hospitals are accountable for implementing strategies to reduce complications by identifying patients who are at risk for developing VTE and implementing strategies to reduce VTE. VTE prevention includes screening for risk, mechanical and pharmacological anticoagulation along with ambulation. Patient and family participation is necessary for effective therapy. There are many barriers to the implementation of each modality throughout the clinical course.
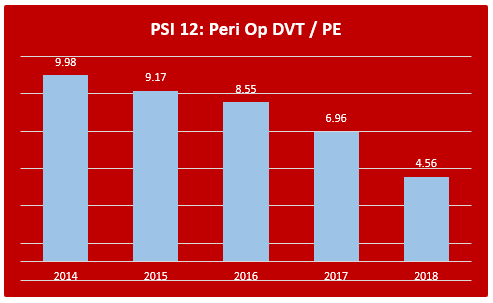
Purpose: The project aims to decrease hospital-associated VTE rates, initially in the surgical population as measured by Patient Safety Indicator (PSI) 12 Peri-operative VTE, to achieve the AHRQ (Agency for Healthcare Research and Quality) benchmark and to implement the program hospital-wide.
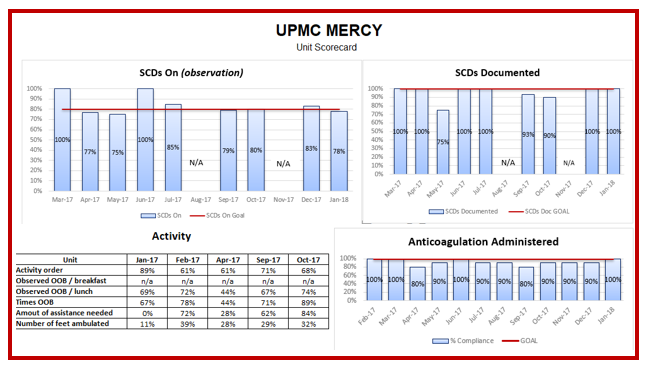
Description: PSIs provide an outlook on patient safety and identifies potentially preventable drawbacks. PSI 12 explores perioperative pulmonary embolism or deep vein thrombosis rates. In our hospital, over half of the incidence in VTE cases were in the postoperative neurosurgical population, followed by the orthopedic population. The neurosurgical patient population was not being provided anticoagulation due to concern for post-op hemorrhage. More current evidence directs anticoagulation safety in the neurosurgical society, and protocols are implemented to begin anticoagulation early in the post-op period. SMAT (standard medication administration times) and missed doses were monitored. A high incidence of patient declination in VTE prevention was noted. Nurses were provided talking points, including focused patient education on admission and escalation to the provider if the ongoing refusal persists. With this engagement, we noticed that patient participation in therapy improved. SCD (sequential compression device) wear time was monitored, discussed during nurse handoff, and documented.Representing professional nurses from each inpatient unit is responsible for the education, implementation, and sustainability efforts of each unit. These responsibilities include training of staff and identifying barriers that are specific to the patient. They work with the unit leader to review all hospital-acquired VTE on their unit and complete point prevalence studies to ensure ongoing compliance. Each unit is provided a scorecard of their VTE rate and process measure compliance.The results, as demonstrated by the PSI 12 graph, show over a 50% decline in perioperative VTE rates in 2018 in comparison to 2014, with the most improvement noted from 2017 to 2018, after the implementation of this project. The unit scorecard reveals the nursing staff is doing an excellent job at SCD documentation. The administration of subcutaneous Lovenox/Heparin was close to our set goal of 100%. Some factors noted to be contributing to the below-par activity level are patient non-compliance to therapy and the clinical condition of these patients. Patient activity level and observation on SCDs are where we see room for further improvement.
Conclusions: VTE prevention requires the participation of both the individual patient and the clinical teams. The process measures anticoagulation administration, SCD wear time, mobility, and patient/family education. Consequently, medical personnel need to provide emphasis to VTE prevention leading to significant morbidity and mortality benefit to a vast patient population.