Background:
Ambulation is significantly reduced when patients are hospitalized, which leads to decreased muscle strength and aerobic capacity. A recent study of geriatric inpatients found daily median step counts of 478 to 846, much lower than the recommended 7,000 to 10,000 a day to maintain cardiovascular and musculoskeletal fitness. Interestingly, daily step count is not associated with admission diagnosis or illness severity, but does correlate with increased mortality post-discharge and 30-day readmission rate. Decreased ambulation can lead to falls, which costs the hospital on average of $11,000 per incident. The Choosing Wisely campaign (American Academy of Nursing) has chosen ambulating elderly patients as a priority to improve quality of care. Few studies have studied ambulation in inpatients, and no studies to my knowledge use activity monitors as a motivational tool to increase ambulation.
Purpose:
To quantify the baseline level of ambulation in our medicine inpatients and increase ambulation through different interventions, with the ultimate goal of decreasing length of stay, 30-day readmission rate, inpatient falls, and discharges to skilled-nursing facilities.
Description:
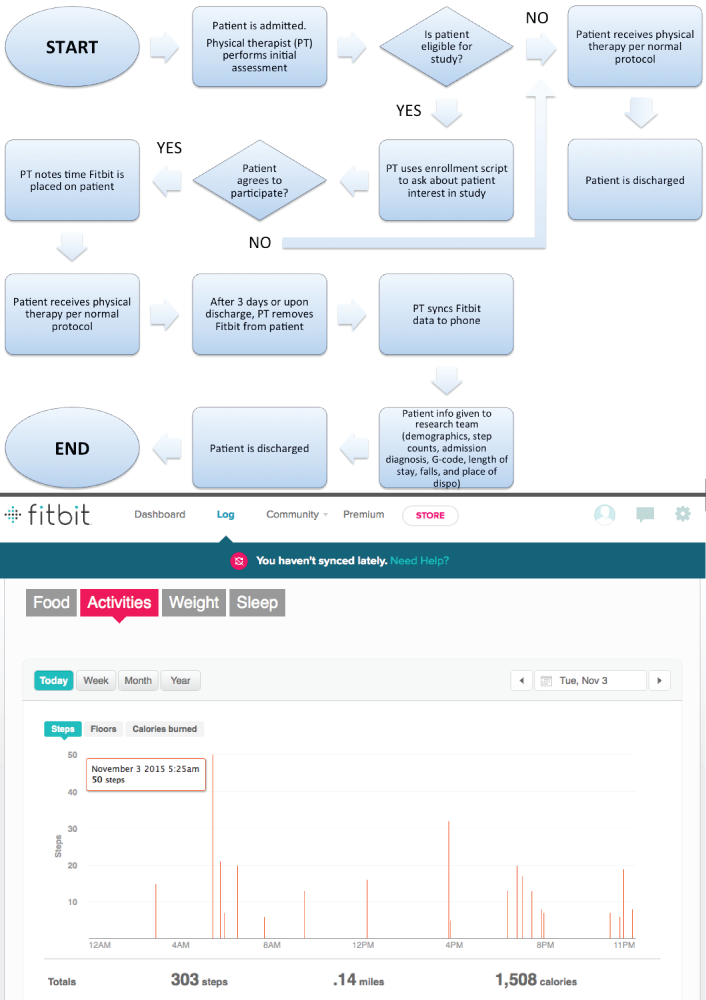
We include medicine inpatients that score between CJ (>20% but <40% impaired/limited/restricted) to CL (>60% but <80% impaired/limited/restricted) on the Activity Measure Post-Acute Care (AM-PAC) scale, a validated scale that measures functional activity. These patients are able to ambulate prior to admission to the hospital, but need some assistance. The physical therapist on the floor then places Fitbits on these patients at the time of her initial assessment.
Our results show that medicine inpatients vary widely in terms of age range, admission diagnoses, and length of stay. The median number of steps per day for patients scoring CJ, CK, and CL, is 488, 303, and 73, respectively. Interestingly, the median number of steps decreased during the hospital stay with 398, 346, and 280 being the respective step counts for day 1, 2, and 3. The next step will involve implementing interventions to motivate patients to ambulate. One such intervention includes providing Fitbits to the medical assistants and having friendly competitions among them to see who walked the most with patients. Other interventions include personalized step count goals for patients and a daily “ambulation hour” on the floor.
Conclusions:
Ambulation in hospitalized patients is significantly lower than the recommended goal, with ambulation decreasing with each subsequent hospital day. Through the use of technology and innovative interventions, we hope to increase ambulation to ultimately decrease 30-day readmission rates, length of stay, and number of falls.