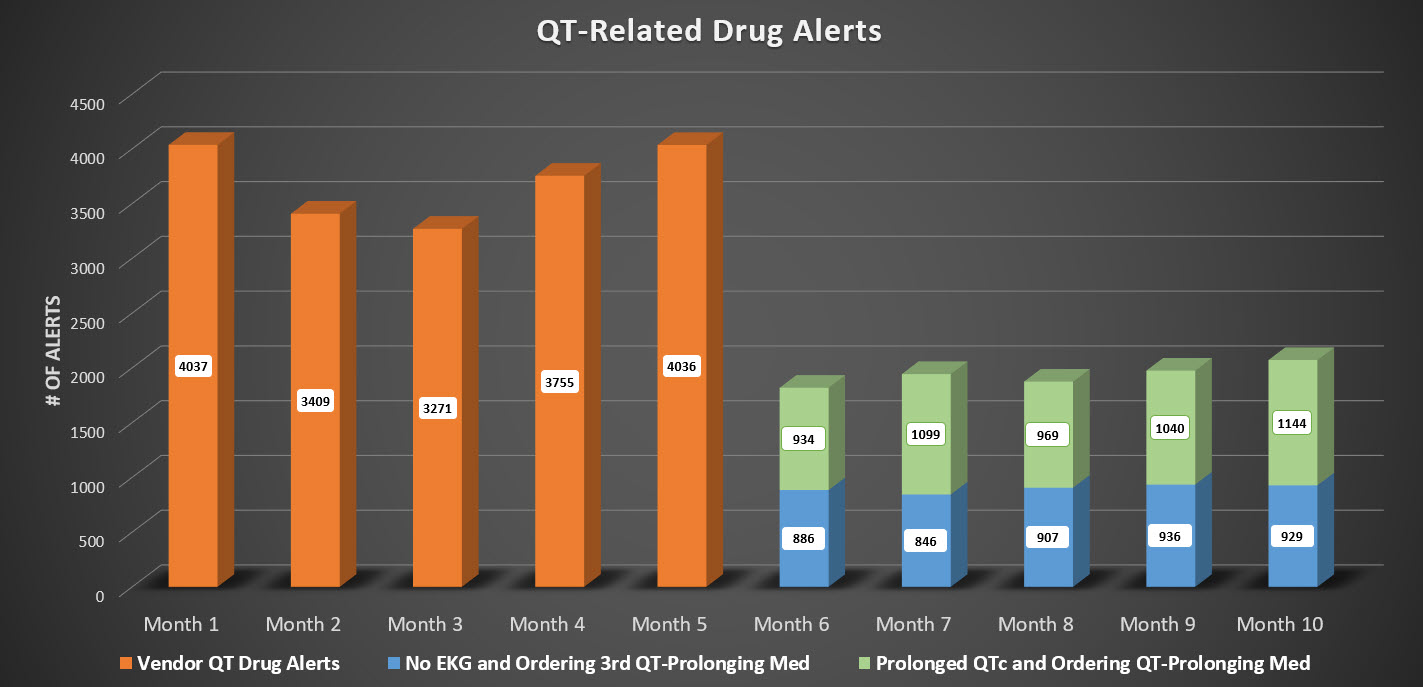
Background: One of the widely reported benefits of electronic health records (EHRs) is the ability to alert clinicians, especially regarding medication-related safety issues. However, soon after the installation of EHRs, the phenomenon of “alert fatigue” was realized. The Agency for Healthcare Research and Quality has shown clinicians override the vast majority of computerized physician order entry (CPOE) warnings. The fear with alert fatigue is that clinicians will learn to disregard alerts in favor of efficiency and will inadvertently overlook meaningful alerts that lead to patient harm. Hospitals with CPOE generally use a vendor to provide drug alert modules to integrate with the EHR. With these modules, QT prolonging medications trigger many alerts. QT-related alerts are in place to prevent the complication of torsades de pointes. Prior to this described innovation, ordering of QT or potentially QT-prolonging medications caused an average of 3701 clinician alerts/month, of which 92% were overridden.
Purpose: The goal of this project was to improve the specificity of QT-related alerts, so that clinicians would be presented with more meaningful data specific to their patient.
Description: Our institution uses Epic EHR and uses First Databank for its drug alert database. Prior to the innovation, there were an average of 3701 QT-prolongation related medication alerts that fired for clinicians each month with a 92% override rate. In lieu of this basic decision support, our team created “smart” decision support that better estimates risk by using data within the patient’s chart. After consultation with our Cardiology team, we created 2 alerts and turned off the default alerts from the drug alert database. One alert is set to fire when a clinician orders a 3rd QT-prolonging medication on a patient who does not have a recent EKG. The second alert is set to fire when a clinician orders a QT-prolonging medication and the patient’s most recent EKG shows a QTc more than 500ms. After this intervention, QT-related alerts fire on average of 1938 times each month, a reduction of 47%. No QT-related patient safety events have been reported since turning off the default QT-related medication alerts.
Conclusions: This innovation describes an approach to addressing alert fatigue by building smarter decision support and seamlessly integrating patient-specific data into clinical decision support. This decision support is able to capture an additional risk (ordering a QT-prolonging medication in a patient with known QT-prolongation), and yet decreased the total number of QT-related alerts. With the continuing advances in interoperability patient-related data is flowing more seamlessly across systems. Clinicians are now needed to take advantage of this technology to build better and smarter decision support tools. The basic decision support logic that is incorporated in current EHRs and alert databases do not capitalize on the wealth of patient-specific data. As we continue advancing EHRs, clinicians, and especially Hospitalists, will be valuable in using this concept to increase the efficiency and effectiveness of clinical decision support.