Background: Syphilis cases in the United States increased by 28.6% between 2020 and 2021. San Francisco was the highest-risk county for early syphilis in 2017, and between 2017 and 2021, syphilis diagnoses further increased by 12%, with a 200% increase in syphilis cases among women and a 333% increase in congenital syphilis cases compared to the prior 5 years. The San Francisco Department of Public Health (SFDPH) recommends syphilis screening in asymptomatic people with risk factors associated with syphilis and in all people who could become pregnant. About 40% of patients admitted to the Internal Medicine resident teams at our urban, safety-net hospital meet criteria for syphilis screening. Despite this, over 50% of these patients with risk factors for syphilis have not received SFDPH-recommended syphilis screening.
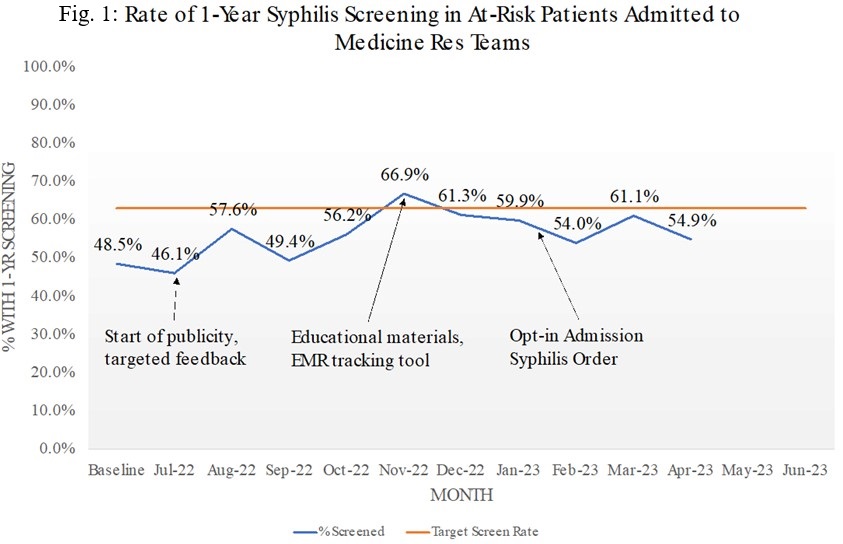
Methods: We initiated an incentive-based quality improvement project to increase syphilis screening in at-risk patients admitted to Internal Medicine resident teams (Medicine, Cardiology, and Medical ICU). Patients with childbearing potential (defined as female sex under age 50 years), homelessness, HIV and/or HCV-infected, and/or active methamphetamine use (defined as urine toxicology test positive for methamphetamines in past 90 days) were considered “at- risk” based on SFDPH guidelines. Our aim was to increase the rate of syphilis screening within one year of admission for at-risk patients to > 63%, an approximate 15% absolute increase from baseline. Beginning August 2022, we provided publicity materials, monthly feedback, and educational resources to the resident teams, along with electronic medical record (EMR)-based tools for tracking syphilis testing history. In January 2023, we launched an updated admission order set that included opt-in syphilis testing. We used binary logistic regression to analyze screening rates during the baseline period (November 1, 2021 to May 31, 2022) and our intervention period (August 1, 2022 to March 31, 2023), adjusting for demographics.
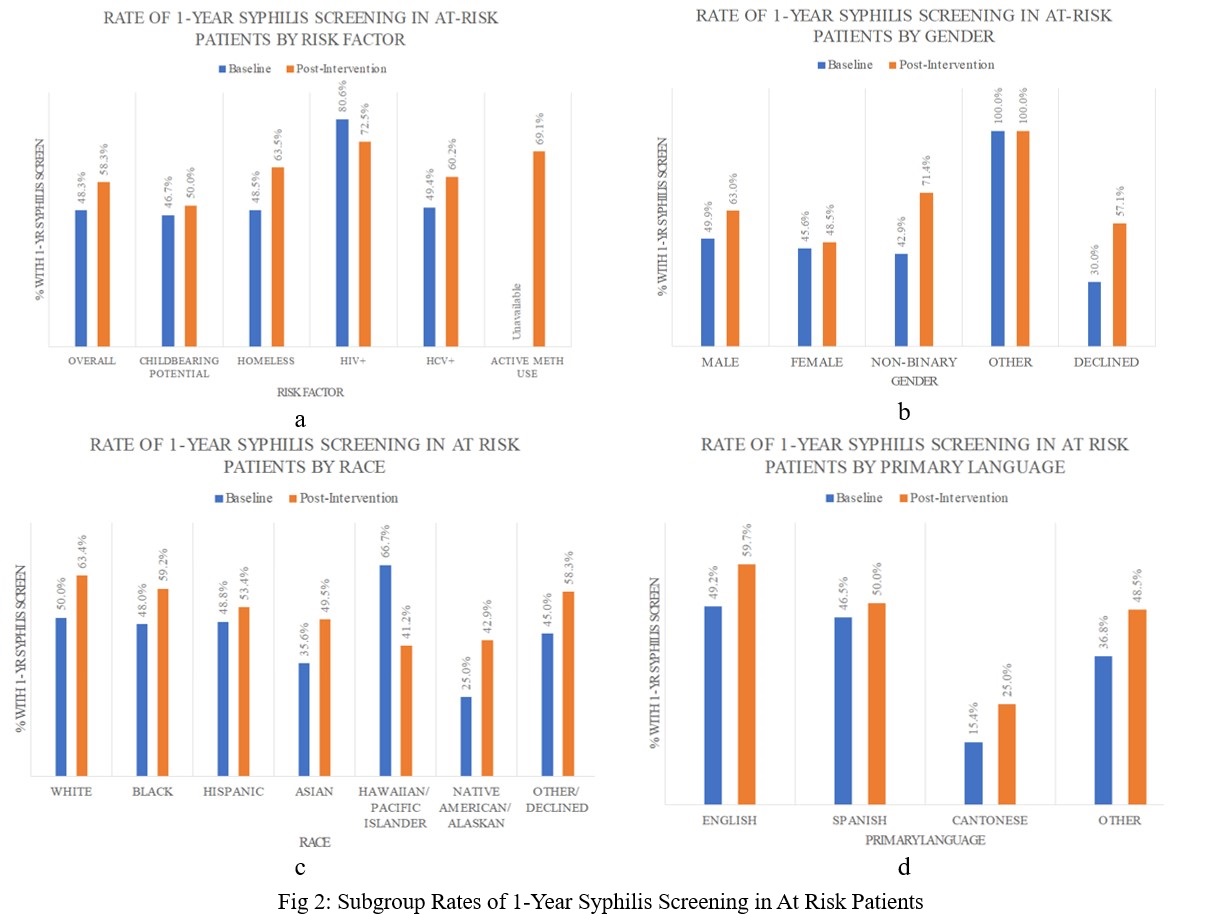
Results: There were 2,140 unique patients (2,609 admissions) in the baseline period and 2,638 unique patients (3,204 admissions) in the intervention period. At-risk patients constituted 39.9% and 44.5% of baseline and intervention admissions, respectively. The average rate of syphilis screening within one year of admission for at-risk patients increased from 48.3% to 58.3% after all interventions, including the updated admission order set (OR 1.39, 95% CI 1.16-1.67, p < 0.01). Syphilis screening rates increased in all at-risk groups, but decreased slightly (80.6% to 72.5%) in HIV-infected patients. Additionally, screening rates improved across all gender, race, and primary language groups with the exception of Native Hawaiian/Other Pacific Islander (n=17). Main reported barriers to syphilis screening included knowledge of screening guidelines, patient acuity, competing care priorities, and high hospital census.
Conclusions: Inpatient admission offers a unique opportunity for guideline-recommended syphilis screening, especially in urban safety-net hospitals. Our combination of education, feedback, and EMR-based interventions significantly increased syphilis screening rates for at-risk patients within one year of admission. Future work should address disparities in screening for at-risk populations, including HIV-infected patients. Follow up studies are needed to ensure appropriate treatment and linkage to care for newly diagnosed syphilis cases detected through inpatient screening efforts.