Background: Advance Care Planning (ACP), palliative care (PC), and enrolling inpatients near end of life into hospice are known methods to improve patient experience and reduce inappropriate use of inpatient (IP) resources. We sought to increase ACP, PC, and hospice referral by proactively identifying patients near end of life.
Methods: In 2020 we introduced the Mandatory Surprise Question (MSQ) as a triage tool for identifying patients who could benefit from ACP. We embedded the question, “Would you be surprised if this patient died within the next six months?” into Hospitalist Division admission order sets. Admitting providers categorized patients as MSQ+ (not surprised) or MSQ- (surprised) based on their response to whether they would be surprised by patient mortality in the next 6 months. We evaluated the utility of the MSQ by comparing mortality outcomes of MSQ+ vs MSQ- patients at various time periods for the first 12 months following the 2020 Hospitalist index IP encounter with the first MSQ response. In 2021 we introduced two dedicated ACP social workers (SW) that interacted with the admitting team before approaching their MSQ+ patients and guiding them through the ACP process. By 2022 we introduced a third SW, and provided CME and other training on ACP, PC, and serious illness communication. In 2021 and 2022 we expanded the ACP program to encompass all major adult inpatient services. We enhanced stakeholder buy-in through institutional goal setting, CME modules, and feedback of ACP program data. PC and Hospice teams proactively approached primary teams about the appropriateness of PC and / or hospice for MSQ+ patients. We tracked mortality, completion of a standardized ACP note, other ACP documentation, referrals to PC and Hospice, conversion of patients with IP status to Hospice, and the Vizient mortality observed to expected (O/E) index. Our hypothesis was that these interventions would drive ACP, referrals to PC and Hospice up while the Vizient Mortality O/E would be reduced. Statistical analyses comparing proportions were performed using the z test statistic with a two-tailed α of 0.05.
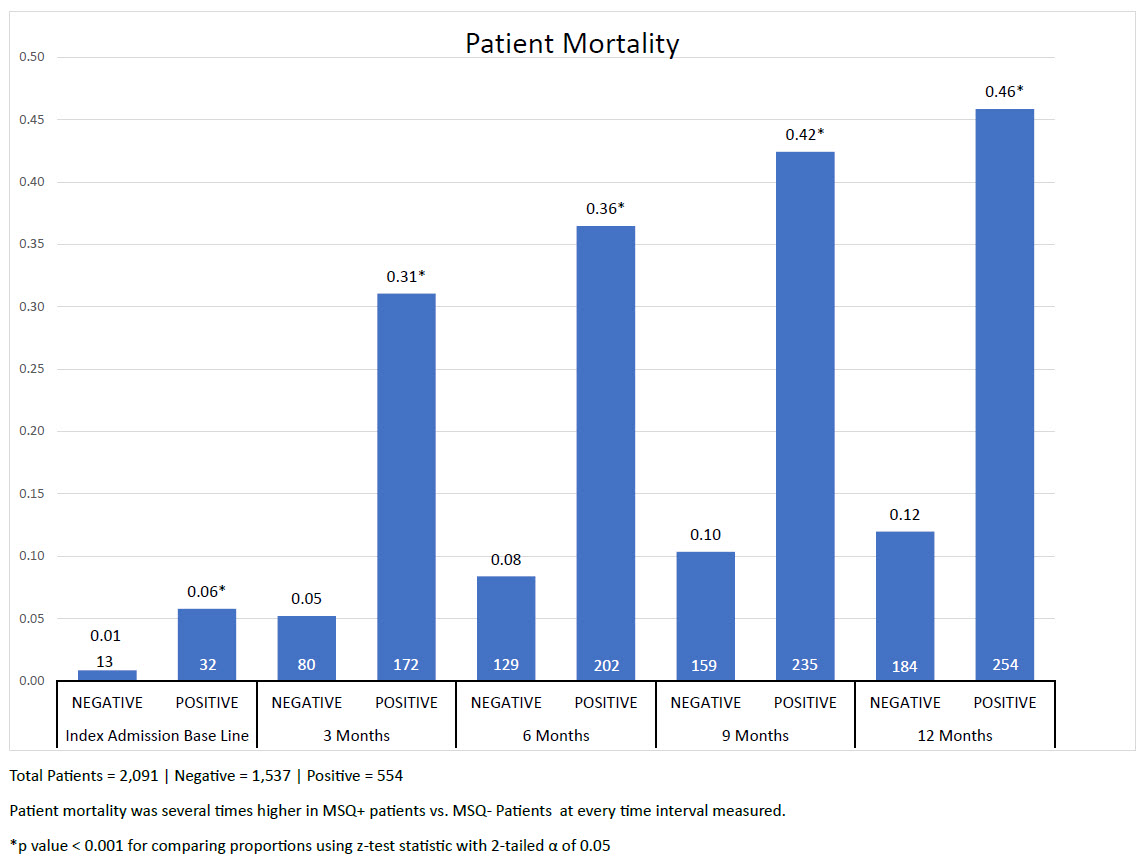
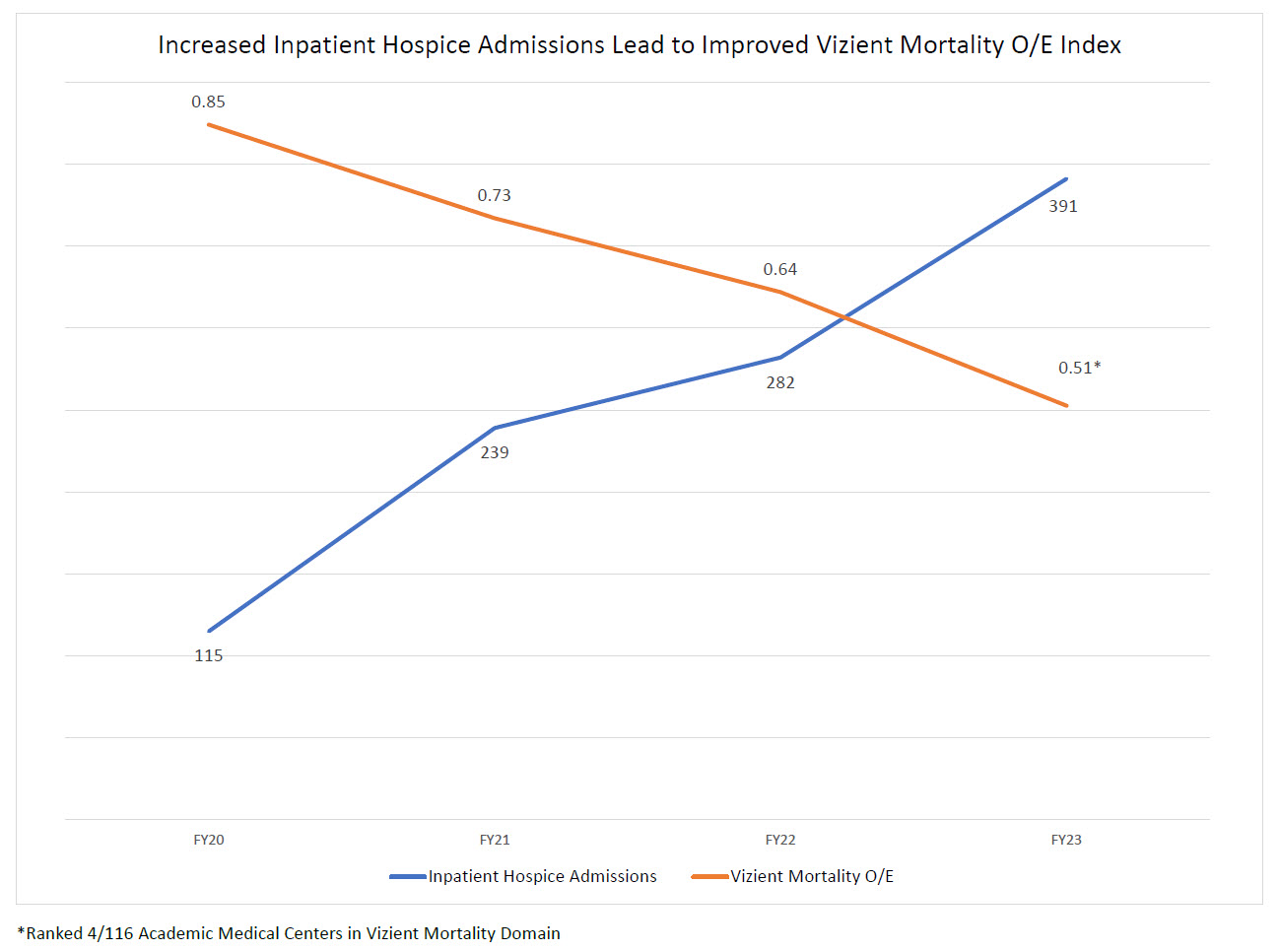
Results: Figure 1. The MSQ proved to be a useful triage tool for identifying patients at high risk of being near end of life. MSQ+ patients were several times more likely to die during the baseline encounter, and at all intervals following the index admission. ACP note completion in MSQ+ patients increased from 60/832 encounters (7.2%) in 2020 to 1507/2366 encounters (63.7%) in 2022 (p < .001). PC referral in MSQ+ patients increased from 199 in 2020 to 622 in 2022, while hospice referral increased from 125 to 505 patients in the same time frame. Figure 2. The number of patients converted to IP Hospice status increased steadily over the years ranging from 115 in FY20 to 391 (240% increase). The organization’s inpatient Vizient mortality O/E decreased from 0.85 in FY20 to 0.51 (40% decrease) in FY23, ranking our institution 4th best out of 116 academic medical centers.
Conclusions: Embedding a simple question (the MSQ) into order sets was well accepted by physicians and effective at triaging patients suitable for SW-assisted completion of ACP, and proactively identifying potential candidates for PC and hospice. Combined with provider training, feedback of data, and regular communication this strategy is a simple, generalizable method to increase ACP, PC, and hospice services for patients aligned with their priorities and wishes, while also reducing unnecessary interventions and reducing healthcare spending.