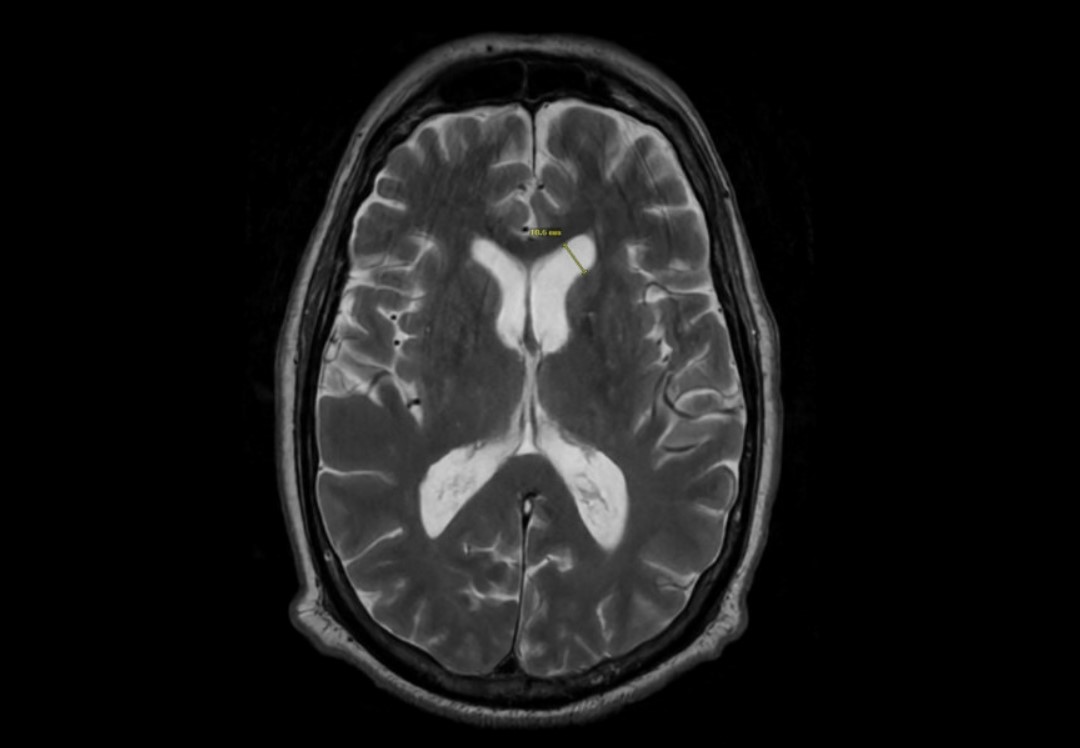
Case Presentation: This case report outlines the case of a 76 year-old male who presented with bacterial meningitis secondary to an infected intrathecal baclofen pump, but initial lumbar puncture cerebrospinal fluid (CSF) did not demonstrate pleocytosis. Patient endorsed worsening headache, vomiting, and bilateral lower extremity weakness 6 days prior to admission. He was immediately started on empiric coverage with vancomycin, ampicillin, and ceftriaxone. He had a brain magnetic resonance imaging which found leptomeningeal enhancements and ventriculitis raising concerns for meningitis. He continued to worsen with development of hallucinations and seizures. He had CSF collected on hospital day 7 and day 11. Initial CSF obtained on day 7 of admission at L4-L5 (delayed due to availability of interventional radiology) demonstrated 1-2 WBC, >600 protein, 132 glucose, negative meningitis/encephalitis panel, negative culture, and eventually negative UCSF metagenomics panel. CSF obtained via direct aspiration of his baclofen pump on day 11 demonstrated 283 WBC, 75 protein, 8 glucose and culture eventually grew pseudomonas. He was discharged on 28 days of ceftazidime after removal of his baclofen pump with recovery back to his baseline.
Discussion: This case highlights the unusual diagnostic course of a patient with 2 weeks of meningitis symptoms and a positive MRI brain who had vastly different CSF profiles due to the method of CSF collection. Lumbar punctures in these cases with intrathecal pumps are notably usually delayed due to the need for interventional radiology to perform the procedure, which subsequently delays diagnosis and treatment of the appropriate organism. There is currently no guideline to suggest that aspirating an intrathecal pump for evaluation of infection is standard of care. This case emphasizes two major learning points; negative CSF studies should not preclude a diagnosis of meningitis if the remaining evidence is highly indicative of meningitis, and early aspiration of an intrathecal pump should be considered for all patients with concern for meningitis to improve diagnostic yield.
Conclusions: In meningitis patients with intrathecal pumps, providers should consider obtaining CSF samples through aspiration of the pump. This case demonstrates that conventional lumbar punctures may not be sufficient to detect a bacterial meningitis due to an infected pump, and lumbar puncture will often require delayed CSF collection with interventional radiology which delays diagnosis and appropriate treatment.