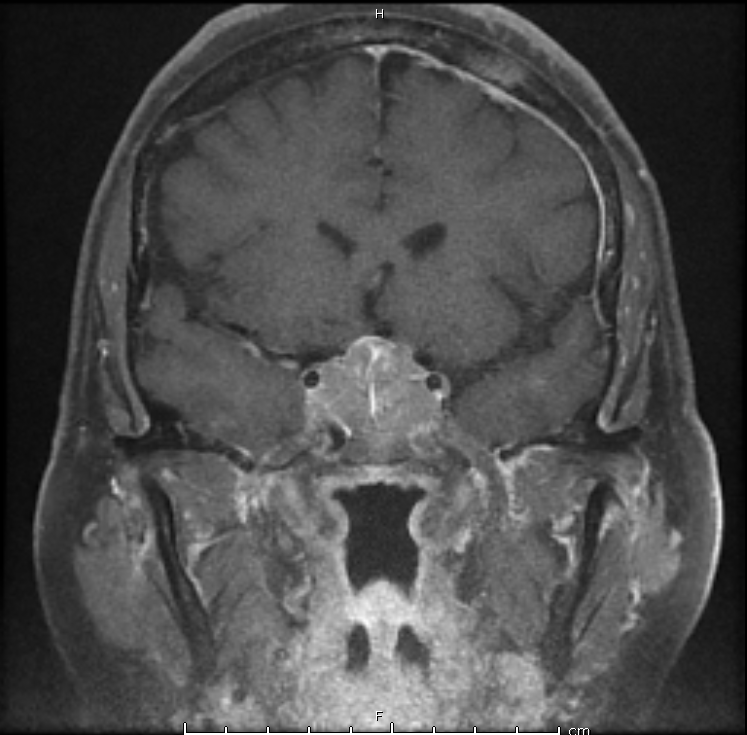
Case Presentation: A 54 year-old female presented to the ED with five days of fatigue, nausea, vomiting, and abdominal pain, increasing confusion, and somnolence after a recent viral illness. On physical exam, she was noted to have large, fixed masses in her breasts with bulky axillary lymphadenopathy. Upon further questioning, the patient revealed that she was diagnosed with breast cancer six years ago prior, but was told by her homeopathic provider that she was cured after her lumpectomy and that her existing breast masses were fibromas. CT scan revealed up to 4-cm enhancing masses in the bilateral adrenal glands. MRI brain revealed a 2.9cm mass invading the posterior pituitary stalk. Subsequent biopsy of a cervical lymph node revealed malignant breast cancer. Initial labs revealed hyponatremia, hypoglycemia, low AM cortisol, and low free T4 with inappropriately normal TSH. Patient was started on hydrocortisone and levothyroxine with improvement of her symptoms. On hospital day 4, the patient reported increased urination. Urine studies revealed immeasurably low urine osmolality and urine sodium, consistent with diabetes insipidus. Her polyuria resolved with initiation of desmopressin. Patient was eventually discharged home with desmopressin, levothyroxine, and hydrocortisone with plans to start chemotherapy and radiation therapy as an outpatient.
Discussion: Breast cancer is one of the most common cancers to metastasize to the pituitary. Metastases to to the pituitary frequently results in pan-hypopituitarism.
The unmasking of central diabetes insipidus may occur by various proposed mechanisms. Glucocorticoid deficiency may increase ADH release through primary secretion from the posterior pituitary and by decreasing water delivery at the renal tubules, which stimulates further ADH release. Increased ADH may also increase translation of aquaporin channels in the renal tubule, preventing diuresis.
After initiation of glucocorticoids for treatment of adrenal insufficiency, providers should have an index of suspicion for diabetes insipidus, particularly if the patient develops polyuria. Patients may not be hypernatremic, such as in this case. Analysis of serum and urine osmolality help confirm the diagnosis. After starting desmopressin for treatment of diabetes insipidus, it is important to monitor serum sodium and urine output.
Conclusions: Providers should be wary of unmasking central diabetes insipidus when initiating glucocorticoid replacement therapy in patients with panhypopituitarism caused by pituitary masses. When the diagnosis of central diabetes insipidus is established, urine output and serum electrolytes should be monitored closely.