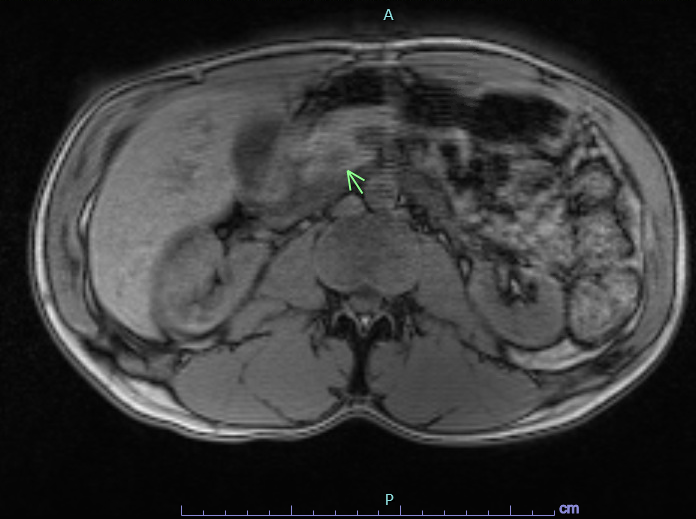
Case Presentation: A 27-year-old male brought to the emergency department after being found unresponsive on the floor. The patient had no recollection of subsequent events until awakening in the ambulance. Notably, he had two prior hospitalizations for episodes of amnesia, “being off” and visual hallucinations. The patient was found to be hypoglycemic by the paramedics with blood glucose level (BGL) of 27 mg/dL and received intravenous dextrose with rapid symptomatic improvement. Clinical examination was unremarkable and history was pertinent for loss of consciousness and urinary incontinence, thus widening the differential diagnoses to include grand-mal seizure, absence seizure, hypoglycemia, substance abuse, and toxins. Initial evaluation showed positive urine toxicology for cannabinoids, normal EEG and non-contrast MRI brain was negative for acute intracranial pathology. Further laboratory workup revealed elevated insulin 34.6 uIU/mL (2.6 – 25.0 uIU/mL) but, interestingly a normal C-peptide of 2.3 ng/mL (0.8 to 3.9 ng/mL) along with negative sulfonylurea testing, normal cortisol level and a BGL of 37. He underwent pancreatic imaging with Dotarem contrast MRI and dynamic contrast-enhanced pancreatic CT which confirmed a 1.5 cm lesion within the pancreatic uncinate without evidence of lymphadenopathy or metastasis. Surgical enucleation of the pancreatic mass was performed with pathology demonstrating a grade 1, well-differentiated, neuroendocrine tumor measuring at 1.5 x 1.4 x 1.1 cm. Immunohistochemistry was positive for CD56, synaptophysin and chromogranin A with Ki-67 proliferative index less than 1% further supporting the diagnosis of insulinoma.
Discussion: Insulinoma is a rare pancreatic tumor of insulin-secreting beta-islet cells and remains the most common cause of hypoglycemia resulting from endogenous hyperinsulinism with approximately four cases per million individuals per year. Patients usually present with classic symptoms of Whipple’s triad and rarely with seizure. This unique case of insulinoma illustrates the diagnostic challenge of symptomatic hypoglycemia with elevated insulin levels and seemingly discordant normal c-peptide. Diagnostic criteria for establishing a biochemical diagnosis of insulinoma revolves around a comprehension of the positive correlation of insulin and C-peptide secretion, especially as C-peptide has a longer half-life. In this instance, the C-peptide level was normal with an elevated insulin level which can devastatingly lead one astray from the critical diagnosis of insulinoma and may in fact lead towards suspicion of surreptitious insulin use. This case aims to highlight the importance of employing the use of molar ratios of insulin to C-peptide. In cases of insulinoma, insulin and C-peptide are at a molar ratio of less than 1 in both the feeding and fasting states as was the case for our patient (Insulin:C-peptide, 0.31), despite initial preconceptions.
Conclusions: Due to the vague presentation and array of differential diagnoses, such tumors can go readily undetected and may present with lethal hypoglycemia. Along with the C-peptide and insulin levels, the molar ratio of insulin to C-peptide must also be considered where insulinoma is suspected in order to achieve an appropriate diagnosis for patients presenting with hypoglycemia. The rarity of insulinomas coupled with a challenging path to diagnosis makes this a true diagnostic dilemma.