Background:
The resident duty‐hour limitations mandated by theACGME increases the number of handoffs of patient responsibility, raising concerns about discontinuity of care and patient safety (Charap, Ann Intern Med. 2004). Meanwhile, the handoff process is left to interns alone in more than one third of training programs (Horwitz et al., Arch Intern Med. 2006). We sought to develop, teach, and supervise a structured, standard method for conducting patient handoffs in an attempt to improve the transfer of information.
Methods:
In July 2005 the Medicine teaching services at Denver Health Medical Center, an academic safety net hospital, were restructured so that all evening handoffs occurred at 1800. After studying and/or directly observing a number of the handoff processes used by several industries and a variety of health care providers, a working group of attendings and residents developed both written and verbal templates for conducting evening handoffs. For the first 4 months of the 2006‐2007 academic year, 2 attendings supervised the handoff process, one for each intern on his or her first night of call. Surveys were designed to determine the interns' perceived skills, attitudes, and knowledge about handoffs, to obtain feedback on perceived optimal frequency and duration of handoffs, and to determine the effectiveness of various aspects of attending supervision. These were administered to each intern on the first day and during the last week of the month‐long rotation.
Results:
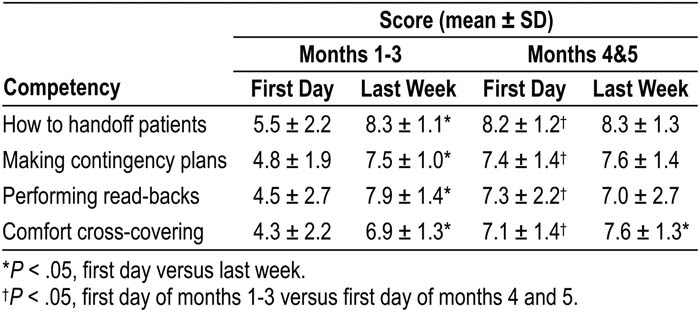
Ninety‐eight percent of the surveys were returned. Eighty‐five percent of respondents thought that attending supervision was “effective” or “highly effective”; 54% and 23% believed that attendings should supervise handoffs for the first 3 or 6 months, respectively; and 76% believed that attendings should supervise the first (38%) or the first and second (38%) call nights of the rotation. Only 51% of interns viewed the didactic/small‐group sessions as effective or highly effective. Other effects of the program are summarized in the table (10‐point Likert scale, with 10 representing “strongly agree”):
Conclusions:
Having a defined handoff process and using a program specifically designed to teach the importance of handoffs and the process by which they should occur is well received and improves interns' self‐assessments of their knowledge about handoffs and their ability to make contingency plans and cross‐cover unfamiliar patients. The first 3 months of the academic year were identified as the period when allocating attending resources to teaching and supervising resident handoffs may have the most benefit. Compared with direct supervision and feedback, didactic sessions about handoffs are relatively ineffective.
Author Disclosure:
E. S. Chu, None; M. B. Reid, None; T. Schulz, None; M. Burden, None; D. Dingwell, None; R. K. Albert, None.