Background: A 2013 Mayo Clinic initiative encouraged proactive communication between physicians and nurses by paging each to bedside for morning rounds, improving physician and nursing perceptions of teamwork. Utilizing a mobile-electronic-health-record-based alert for such a process may reduce implementation costs and feasibility barriers. Previously, we piloted an updated interprofessional bedside rounds (IBR) model that utilized secure-texting platform alerts to improve attending, resident and nurse communication on select general medicine services and units at an academic hospital. These initiatives led to increased self-reported physician and nurse satisfaction with team communication. It was restricted, however, to volunteer hospitalists and three hospital units closely affiliated with hospitalists. Given many quality improvement projects fail to scale, our primary objective was to explore the scalability of expanding the IBR model to the entire Division of Hospital Medicine, involving a more varied range of clinician teams and units.
Methods: Participants included all hospitalist attendings and advanced practice clinicians, the residents on general medicine teams, and nurses for patients on 11 hospital medicine services across 13 units at a single, urban academic teaching hospital between 4/2024 and 6/2024. A multidisciplinary executive committee developed and communicated process expectations via email, secure-texting platform, and in person. To engage in IBR, the medical team sends a secure-text to alert the primary nurse to bedside rounds. The medical team then prompts the nurse to advise regarding (1) any questions/concerns and (2) any orders needed, and (3) the medical team informs the nurse of the plan for the day. Participants were surveyed before and after the intervention across twelve domains using a 5-point Likert scale: team-nurse communication satisfaction, medical plan knowledge, burden of post-rounds unnecessary communications and orders, and the six-question Safety Attitudes Questionnaire (SAQ).
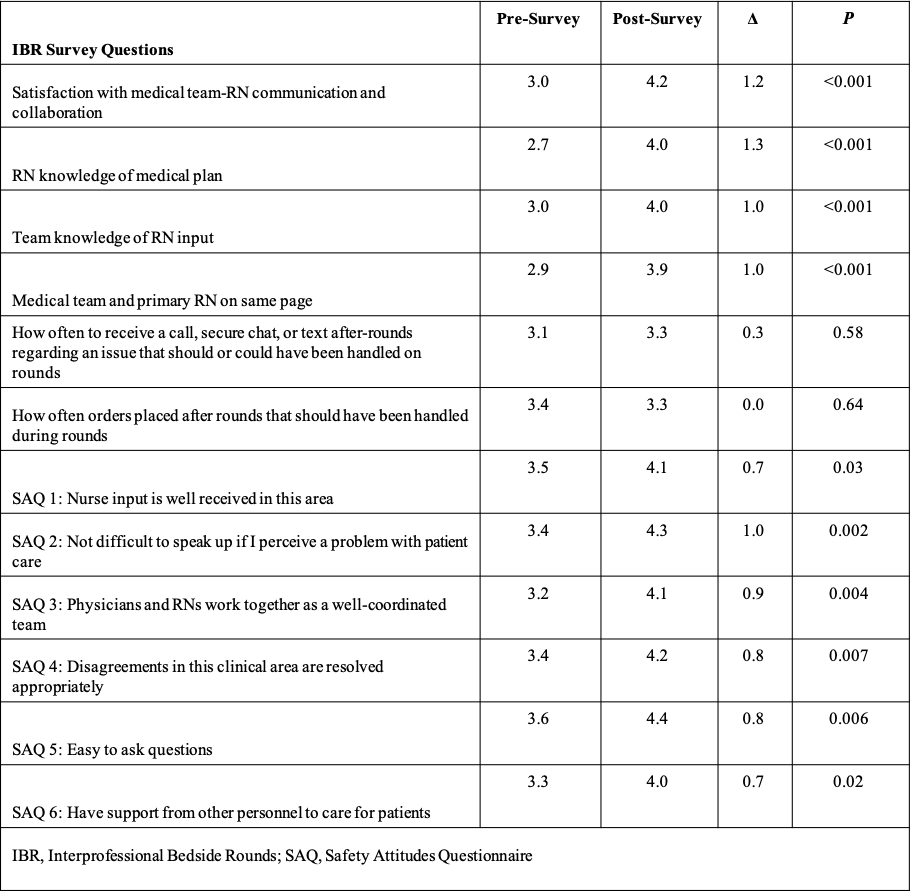
Results: Using matched pre-post survey analysis (42% [44/104] post response rate), 11/12 domains showed trends toward improvement (10 were significant) (Table 1). The average pre-post response increased from 3.2/5 to 4.1/5. Satisfaction with medical team-RN communication and collaboration increased 1.2 (p< 0.001); RN knowledge of medical plan 1.3 (p< 0.001); team knowledge of nursing input 1.0 (p< 0.001); team and nurse are on the same page 1.0 (p=0.001); SAQ-nurse input well received 0.7 (p< 0.03); SAQ-not difficult to speak up 1.0 (p=0.002) SAQ-physician-nurses work together as a well-coordinated team 0.9 (p< 0.004); SAQ-disagreements are resolved appropriately 0.8 (p=0.007); SAQ-easy to ask questions 0.8 (p=0.006); and SAQ-have support from other personnel to care for patients 0.7 (p=0.02), respectively.
Conclusions: Expansion of IBR through EHR-based notification to all Hospital Medicine units and teams was effective in enhancing clinician and nursing communication and satisfaction. We were able to demonstrate the scalability of IBR while maintaining the positive impact. The final step will be to assess the sustainability of this process.