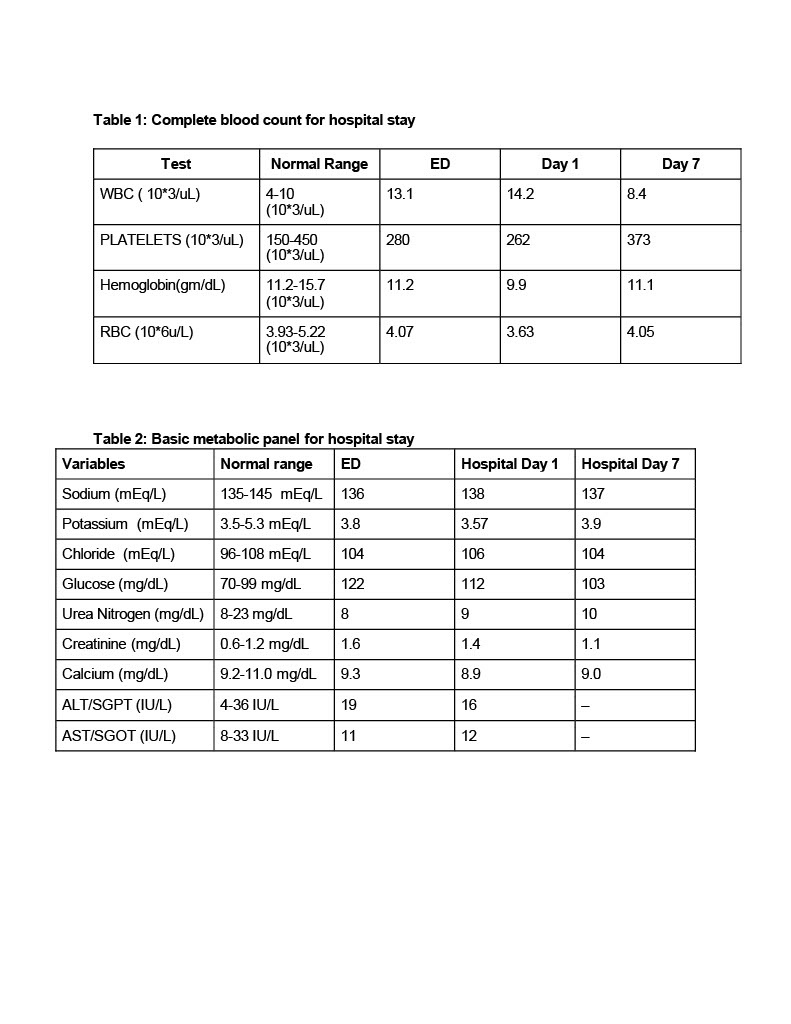
Case Presentation: A 45-year-old female presented with fever, chills, bilateral flank pain radiating anteriorly and intermittent right upper quadrant pain prior to arrival. Medical history included hypertension, stage 3a chronic kidney disease, obesity, uterine fibroids, and treated Helicobacter pylori infection. Her vitals were as follows: 98.6 °F, heart rate 126 beats/minute, respiratory rate 20 breaths/minute, oxygen saturation 98% on room air, and blood pressure 90/60 mmHg. Physical exam was unremarkable except for mild left lower quadrant tenderness. Labs showed leukocytosis with neutrophilia, normocytic anemia, elevated creatinine of 1.6, and a urinalysis without pyuria (Table 1 & 2). Due to concern for sepsis, blood and urine cultures were obtained, and empiric antibiotics were started. On day 2, blood cultures grew Haemophilus influenzae (Hib), and antibiotics were narrowed to ceftriaxone. She had no signs of meningeal involvement, and her neurological status remained stable. To attribute a source, the workup included a chest X-ray, which was negative for infection, an US of the gallbladder showed sonographic Murphy sign but HIDA scan ruled out cholecystitis (Figure 1 & 2), and a transvaginal ultrasound showed fibroids with no other abnormalities. Transthoracic and transesophageal echocardiograms ruled out endocarditis. Complement studies were ordered to rule out risk factors for Hib invasive disease and ANA, C3, and CH50 were negative. She tested negative for HIV. Repeat blood cultures were negative, and she improved clinically. She did not present with or develop any respiratory symptoms. She was discharged on cefuroxime to complete a 14-day course and was vaccinated for Hib prior to discharge.
Discussion: Haemophilus influenzae, a Gram-negative coccobacillus, is a common pathogen in children but may cause invasive disease in adults. While serotype b (Hib) is most pathogenic, non-typeable Haemophilus influenzae (NTHi) has emerged as a leading cause of invasive disease in adults. Bacteremia is typically secondary to respiratory tract infections such as pneumonia, sinusitis, tracheobronchitis, and epiglottitis although rarely, cholecystitis, endometritis, infections of the urogenital tract, and cellulitis have also been implicated. Less common forms of invasive Haemophilus influenzae disease include endocarditis, pericarditis, septic arthritis, and osteomyelitis [5]. The patient’s history of uterine fibroids raised suspicion for a gynecological source, but imaging and exam was negative. Gallbladder disease was also ruled out. No primary source of infection was found, despite a comprehensive work up. We ruled out possible sources of infections as reported in the literature as well as individual risk factors such as immunocompromised states, sickle cell disease, asplenia, and complement deficiency syndromes. Such individuals are at risk because encapsulated organisms require clearance by complement proteins and a functional spleen [5]. Although an occult respiratory tract colonization is a possible explanation of bacteremia, the lack of a clear source is consistent with literature reporting cases of Haemophilus influenzae bacteremia without a definitive focus.
Conclusions: This case underscores the importance of considering Haemophilus influenzae in sepsis cases with no clear focus of infection, illustrating the diagnostic challenge invasive disease may present, emphasizing the need for further research on its epidemiology and resistance patterns in adults.