Background: During COVID-19, students, residents and their programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation.
Purpose: One increasingly available tool that can help protect trainees, preserve personal protective equipment (PPE), while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our students and residents rotating at a large community hospital (affiliated with the area medical school) we have used video visits to continue our mandate as both healthcare and education professionals.
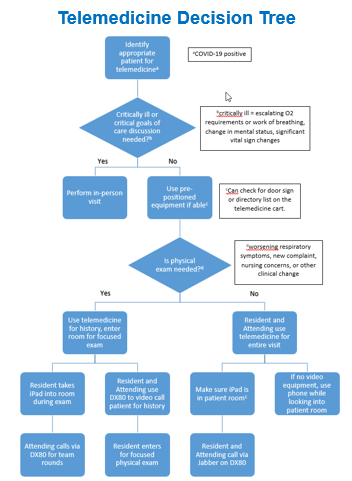
Description: We implemented and assessed a telemedicine virtual rounding program to supplement traditional rounding for learners on inpatient teaching teams. Step one was training of a framework for telemedicine use (virtual rounding with patients and attending). Step two was implementation of telemedicine in internal medicine rotations using a decision tree (see supplemental figure). Step three was evaluating the innovation via surveys provided at the end of rotations. 17 medical students and residents participated in the pilot program from June-September, 2020. Telemedicine was used a total of 82 times with 77% (n=63) involving virtual rounding with the team and the patient and 19% (n=23) involving virtual rounding with the team and attending. Free-text responses coded into four thematic groups described what learners found valuable in the telemedicine experience: 1) Information Gathering: Learning to obtain pertinent information virtually +/- physical exam (teledevices or via telesupervision); 2) Webside Manner: Learning to navigate the virtual sphere, understand telepresence, and optimizing verbal and nonverbal communication skills; 3) Technical Proficiency: Gaining proficiency with telemedicine platforms and applications; 4) Awareness of Health Disparities: Exploring creative solutions for patients, particularly those that suffer from baseline health care disparities.
Conclusions: Prior to the COVID-19 pandemic, telemedicine adoption was limited due to lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. Telemedicine should be a developing part of the education and training for healthcare learners. Ensuring that the growth of telemedicine does not worsen disparities in care is also essential. This pandemic has underscored the need for providing telemedicine services that will outlast this crisis and to support our healthcare learners in being effective on our care teams.