Background: While delirium may affect patients of any age, delirium prevention and management protocols have focused mostly on the elderly, as older adults (>65 years old) are more vulnerable to developing delirium. Delirium has been reported in 19-31% of younger adults during their hospital stay, and 15-56% of older adults.There is lack of literature on delirium in younger adults. In this study, we assess the differences between younger (18-65 years) and older adults (>65 years) who were diagnosed with delirium during their hospital stay, using a large population health database between 2003 and 2017.
Methods: Data for this study was obtained from Optum Clinformatics™ Data Mart (OptumInsight, Eden Prairie, MN). The Clinformatics™ Data Mart is a database comprised of administrative health claims for members of a large national managed care company affiliated with Optum and members with Medicare Advantage with Part D coverage. It includes a geographically diverse population of approximately 15-18 million annual covered lives.3,458,765 adult patients who were diagnosed with delirium during their hospital stay and discharged from the hospital between December 31, 2003 and December 31, 2017 were included. Delirium was identified using International classification of disease (ICD) diagnosis codes (not present on admission).Bivariate analysis was conducted to assess the differences between younger (18-65 years) and older adults (>65 years) who were diagnosed with delirium during their hospital stay.
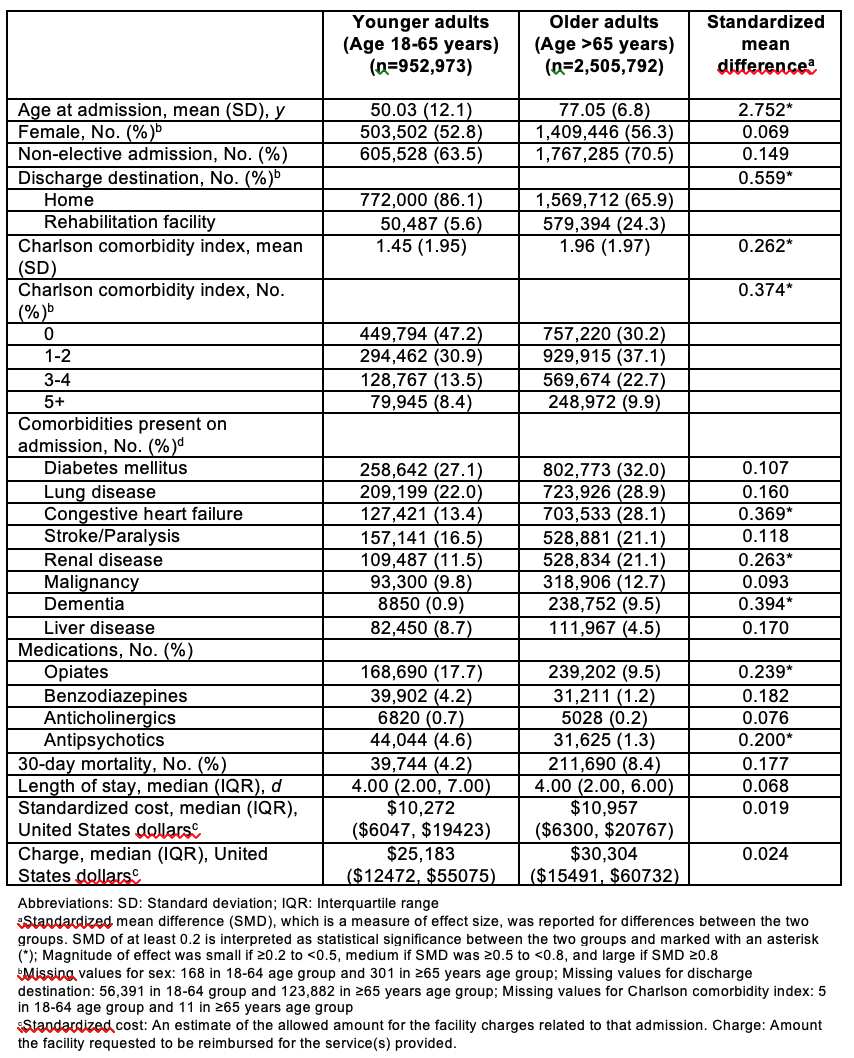
Results: 27.6% of the patients who were diagnosed with delirium during their hospital stay, were younger adults (Table 1). Majority of the patients with delirium in either age group had a non-elective admission to the hospital. Younger adults with delirium were more likely to be discharged to home after the hospitalization (86.1%) compared to older adults with delirium (65.9%). 5.6% of the younger adults with delirium were discharged to a rehabilitation facility compared to 24.3% of the older adults with delirium. Younger adults with delirium were more likely to have received opiates (17.7% versus 9.5%) and antipsychotics (4.6% versus 1.3%) compared to older adults with delirium but there was no significant difference in the use of benzodiazepines or anticholinergics.Mean Charlson comorbidity index was 1.45 ± 1.95 for younger adults with delirium compared to 1.96 ± 1.97 for older adults with delirium. The most common comorbidities among younger adults with delirium were diabetes mellitus (27.1%), lung disease (22.0%), stroke (16.5%), congestive heart failure (13.4%), and renal disease (11.5%). The most common comorbidities among older adults with delirium were diabetes mellitus (32.0%), lung disease (28.9%), congestive heart failure (28.1%), renal disease (21.1%), and stroke (21.1%). Older adults with delirium were more likely to have dementia (9.5% versus 0.9%) and renal disease (21.1% versus 11.5%) compared to younger adults with delirium.30-day mortality was 4.2% for younger adults with delirium compared to 8.4% for older adults with delirium but the difference was not statistically significant. There was no significant difference in the median length of stay or cost between younger and older adults with delirium.
Conclusions: Most delirium initiatives in hospitals are restricted to older adults but the burden of delirium among younger adults was nontrivial at 27.6%. Younger adults with delirium may have similar 30-day mortality, LOS and costs during their hospital stay as older adults.