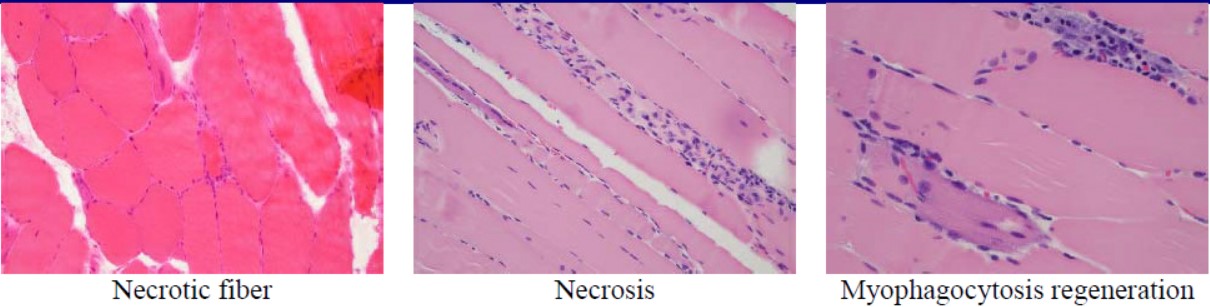
Case Presentation: A 51-year-old Caucasian male presented for evaluation of worsening lower extremity muscle weakness and associated myalgias. He received a diagnosis of NAM after three months of progressive proximal, symmetric upper and lower extremity weakness with myalgias, and an initial creatinine kinase (CK) of 13,875 IU/L. He had been on Atorvastatin 40 mg for five years, discontinued when statin-induced myopathy was suspected one month before admission to the hospital with worsening proximal muscular weakness and diagnosed with non-traumatic rhabdomyolysis. Workup on admission showed positive serum anti- HMGCR antibodies > 200 units done, electromyography (EMG) with the presence of an irritable myopathy with complex repetitive discharges, and a left biceps brachii biopsy with necrotizing myopathy and negative MHC class I antigen expression. A myositis antibody workup included SSA-52, SSA-60, PL-7, PL-12, Mi-2, Ku, EJ, OJ, Ribonucleic protein antibody (U1), Jo-1 antibody, and anti-signal recognition particle (anti-SRP) antibody which were negative, and computed tomography (CT) of chest, abdomen, pelvis did not show any malignancy. He was started on prednisone 60 mg daily. CK levels were 7,900 IU/L after two weeks of therapy; however, muscular weakness persisted. One week later, he presented with progressive proximal weakness, worse in lower extremities, requiring assistance for most daily life activities. CK was 10,807 IU/L. He was started on 1 mg of intravenous (IV) methylprednisolone for three days and then 48 mg of oral methylprednisolone daily. He underwent four total treatments of plasma exchange occurring every other day. Muscle strength improved, and CK level 4,344 IU/L after the therapy. He currently is starting monthly intravenous immunoglobulins (IVIG) with a steroid taper with incomplete resolution of muscular weakness: arm abduction of 4/5 and a hip flexion of 2/5 using the medical research council (MRC) scale and a CK level of 2,651 IU/L
Discussion: Our case represents the challenging management of patients with NAM with persistent muscular weakness and high creatine kinase over several months. This entity represents a differential diagnosis to consider in patients with proximal muscle weakness with or without a history of statin use, as exposure to the drug is not required, with some case series reporting up to 55% of patients not exposed to it. Therapy can vary, as most of the cases described have needed more than one immunosuppressive therapy to achieve clinical improvement5, and few described the use of plasmapheresis. Up to 50% of patients will achieve full strength at two years. Younger patients tend to have more severe disease and worse prognosis, and there has been association with a predisposing genetic component. Our case showcases a rare entity associated with a common drug in hospitalized patients. Future research will need to be guided to identify adequate therapies, either as monotherapy or combination treatment for this disease.
Conclusions: Statin-induced necrotizing autoimmune myopathy (NAM) is a rare disease associated with the use of statins and the presence of 3-hydroxy-3 methylglutaryl coenzyme A reductase antibodies (HMGCR). Patients present with proximal muscular weakness, elevated creatinine kinase (CK) and biopsy findings of necrotizing myopathy without inflammatory infiltrate. Patients do not need to have been exposed to statins for which this pathology should be included in differentials of proximal weakness as a muscle biopsy can be diagnostic.