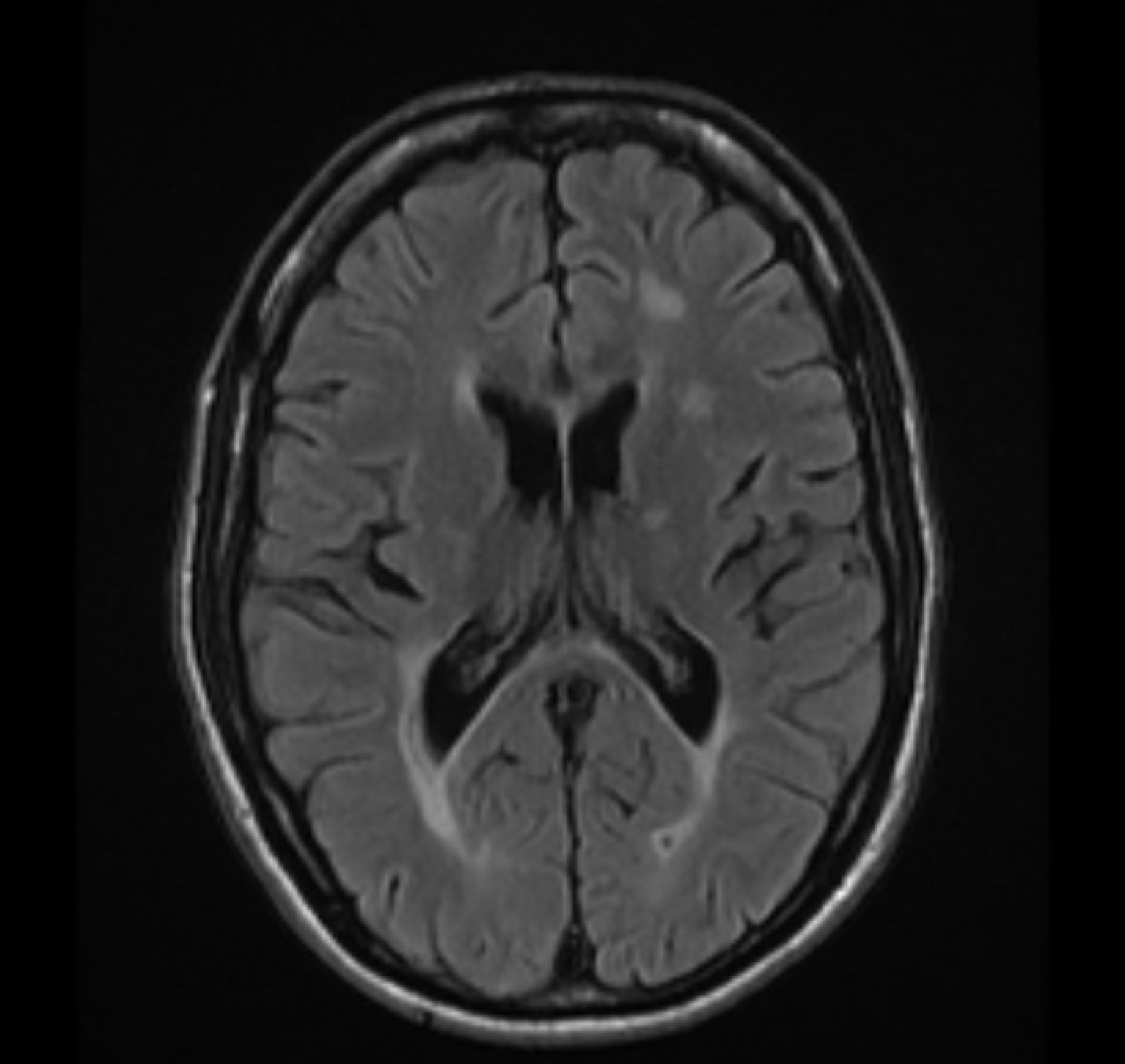
Case Presentation: 41 years old Hispanic gentleman with no significant past medical history who presented to the hospital for difficulty walking and diarrhea.Over the last four years, he has had watery non-bloody diarrhea multiple times daily. He reported one bloody bowel movement a week before his presentation. He had lost a significant amount of weight despite a good appetite.Regarding his difficulty walking, it started about two years before his presentation and was progressive in nature, his legs felt heavy and numb, his walking acutely worsened two months before his presentation, he denied any further symptoms. Physical examination showed a cachectic patient with temporal wasting and a benign abdominal examination, neurological examination demonstrated bilateral lower extremities weakness involving hip, knee, and ankle (left side more than the right), hyper-reflexia of bilateral patellar jerk and bilateral extensor plantar response, decreased vibration and pinprick sensations bilaterally up to 8 centimeters above the ankles, with intact remaining neurological examinations. Initial workup showed CRP of 1.8, MRI of brain and spine demonstrated the advanced demyelinating process in the brain, mid and lower C spine level of the spinal cord, suspicious for multiple sclerosis, without abnormal enhancement. CSF demonstrated RBC of 3, Glucose of 70, WBC of 0 and protein of 53 with IgG oligoclonal banding (CSF IgG index of 1.5, the normal range is 0-0.7), based on MacDonald criteria, he was diagnosed with primary progressive MS. At the same time, Colonoscopy and EGD with biopsies were done that confirmed the diagnosis of ileocolonic Crohn’s disease. The patient was immediately started on high dose IV pulse steroid for 5 days then transitioned to oral therapy, he had a very quick and remarkable improvement of his weakness and diarrhea.
Discussion: The association between multiple sclerosis (MS) and inflammatory bowel disease (IBD) has been suggested multiple times in the previous literature, not only from their common immunological patterns but also due to observations of increased incidence of both IBD among MS patients and MS among IBD patients1. We are presenting a rare case of a gentleman who presented with chronic diarrhea and lower extremities weakness, who has been diagnosed simultaneously with both MS and Crohn’s disease (CD). An association between MS and IBD has been suspected for decades2. The estimated prevalence of MS in the general population is about 0.1%, while in IBD patients the prevalence of MS has been reported at up to 0.5%3, suggesting a 1.5-5-fold increase in the risk4. MS has been reported to develop either before or after the clinical onset of IBD5. The nature of a possible pathogenic link between these two entities has not been identified, but a disturbance in functional T-cell subsets with the aberrant pro-inflammatory activity of T helper 17 subsets has been suggested6.
Conclusions: Hence, due to this possible association brain MRI followed by a neurological consultation for further diagnostic workup should be organized as soon as a patient with a clinical history of IBD presents with a neurological symptom suggestive of MS.