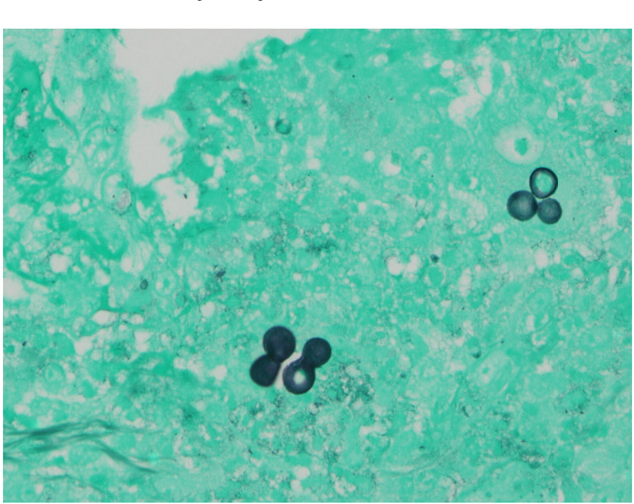
Case Presentation: A 22-year-old male with a history of substance abuse presented with a non-healing wound to the right lateral ankle. The wound began as a blister several months prior and had been worsening. Review of systems was negative for fever, chills, cough, fatigue, malaise.Physical examination was significant for a 5 cm annular hyperpigmented fungating mass at the right lateral ankle with a 1 cm satellite lesion inferiorly, without any active discharge (Figure 1). Labs showed a normal WBC count. MRI of the ankle showed a thin fistulous communication to the skin surface where there was a plaque-like fungating skin mass extending about 5 cm. There were superficial lateral malleolar erosive changes involving the lateral and posterior aspect of the malleolus. The findings were concerning for the possibility of aggressive skin malignancies such as cutaneous squamous cell carcinoma and melanomaDermatology performed shave biopsies that showed broad based budding yeast forms suggestive of Blastomycosis on Grocott’s Methenamine Silver (GMS) stain (Figure 2). Later, blastomycosis antigen was detected in blood. The patients’ wound improved with liposomal Amphotericin B. Unfortunately, he developed acute kidney injury with very slow renal recovery, so he was transitioned to itraconazole with plans to continue therapy for 6-12 months. A CT chest/abdomen/pelvis to rule out further fungal involvement was negative. Immune status workup was also negative for any abnormalities.
Discussion: Blastomycosis is a systemic infection caused by inhalation of B. dermatitidis and B. gilchristii. Infection is most often found in the lungs (91 %) but can also be seen in skin (18 %) and bone (4%). Extrapulmonary involvement arises from hematogenous spread from primary pulmonary infection. Though definitive diagnosis requires growth of the organism from specimens of the affected site, presumptive diagnosis with direct visualization methods justifies starting empiric antifungal therapy. These methods include wet prep, using calcofluor white and/or KOH stains, and histopathologic examination with (GMS) stain. Under microscopic examination, Blastomyces are easily differentiated from others on the basis of their size (8 to 15 microns in diameter), and single, broad-based buds. Serologic testing, Nucleic Acid Amplification, and Antigen testing are available for diagnosis and treatment response. However, their use is limited due to low sensitivities, cross-reactivities with other endemic fungi, and because easier and more cost-effective methods are available. Itraconazole is recommended to treat patients with mild to moderate severity disease. For patients with moderately severe to severe disease (pulmonary or extrapulmonary), initial therapy with amphotericin B is recommended followed by itraconazole. Severity depends on site involvement, extent of involvement and immune status.
Conclusions: Although invasive fungal infections are typically seen in patients with compromised immunity, Blastomyces is unique in its ability to infect both immunocompromised and immunocompetent hosts. Lung involvement is most common but skin disease and bone disease are the next most common extrapulmonary sites of infection as seen in our patient. Definitive diagnosis requires culturing the organism from clinical specimen but tissue examination is crucial for rapid diagnosis and start of treatment!