Case Presentation:
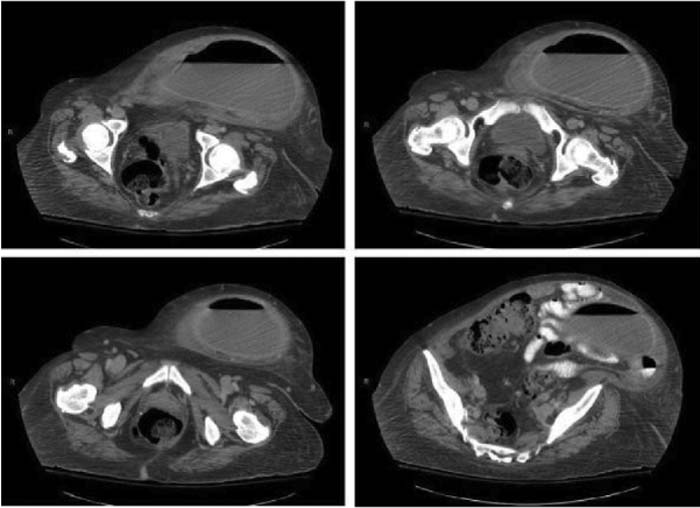
A 51‐year‐old woman with a medical history of congestive heart failure, hepatitis B, and hypothyroidism was transferred from an outside hospital for a workup of an abdominal mass. The patient had presented several months ago to her parent facility complaining of abdominal pain and swelling. A workup performed at the referring facility revealed significant abdominal ascites without evidence of overt heart failure. She underwent serial large‐volume paracentesis, which revealed a transudative fluid with benign cellular elements. The patient underwent an abdominal CT scan that confirmed the presence of ascites but also revealed scattered diverticuli and a 10‐cm cystic pelvic mass. As her liver appeared heterogeneous in texture on CT, an ultrasound was performed that showed no focal masses or biliary dilation, A liver biopsy was performed that was negative for malignancy but did reveal chronic hepatitis. An urgent colonoscopy was also performed that showed no primary colonic malignancy. A subsequent PET scan showed increased activity over this mass and diffusely throughout the peritoneum, worrisome for peritoneal carcinomatosis. The patient was told she had metastatic ovarian cancer and was transferred to our facility for further intervention. On arrival to our institution, the patient underwent repeat abdominal imaging (Figure 1). Tumor markers were sent, and a CA‐125 returned abnormal at 75 U/mL (0‐35 U/mL). All other tumor markers were negative. A transvaginal ultrasound confirmed a cystic mass but was unable to confirm confluence or origin of this structure with the adnexae. Thus, a CT‐guided aspiration with drain placement was performed. The aspirate was negative for malignancy; however, subsequent bacterial cultures grew Streptococcus, Milleri, and Bacteroides species. Review of imaging studies suggested a “nippling” of the cystic mass toward the region of the cecum, confirming a contained abscess from a microperforation.
Figure 1. CT demonstrating focal microperforation within the midsigmoid colon with what appears to be a tract extending from this region into the collection suggesting an abscess.
Discussion:
This case illustrates the importance and occasional extreme difficulty of obtaining tissue to confirm the diagnosis of malignancy. Whereas the patient underwent multiple appropriate interventions to better elucidate the nature of this cystic mass, no single test confirmed the diagnosis. It was only when a transvaginal ultrasound did not show an obvious connection with the ovaries that other diagnostic entities, including those of a contained perforation with abscess formation, were entertained. The patient's PET scan was obviously positive in this hypermetabolic, infected region. Her abdominal ascites was likely explained by a combination of cirrhosis, volume overload, and localized infection.
Conclusions:
An open and keen diagnostic differential is key to the appropriate workup of any abdominal mass. Benign entities should never be ruled out unless conclusive tissue diagnosis suggests otherwise. Our patient is scheduled to undergo a curative resection of this abscess, completely changing her original bleak prognosis and outcome.
Author Disclosure:
V. Chopra, none.