Case Presentation: A 77 year old man with adenocarcinoma of the lung s/p chemotherapy and radiation presented to the Orthopedics service with hip pain & a left femoral lytic lesion.Soon after his IR-guided femur biopsy, medicine consult was called for ? cellulitis. Patient had new left 2nd toe pain, ankle pain, & knee pain, with rapidly progressing redness over the ankle and toe (figure 1). Denied history of similar pain, no history of gout.
Uric acid normal at 6.1, WBC 7.1, Elevated CRP to 138.4. Arthrocentesis of the ankle showed WBC of 444 cells/mm3 with 63% PMN. Gram stain negative for bacteria. No crystals seen.
Patient had recently started Durvalumab therapy and was 7 days s/p his 3rd dose (dosed q 2weeks, day 35 of therapy.)
Rheumatology consult recommended checking ANA, HLA B27, anti-CCP, and RF – all negative. They also recommended Prednisone, 20mg tapering down to 10mg over 9 days.
Pt experienced rapid resolution of symptoms.
At the time of this report, patient has received two additional cycles of Durvalumab without recurrence of arthritis.
Discussion: Immune checkpoint inhibitors (ICI) have revolutionized treatment for certain cancers. Durvalumab is an ICI that prevents T cell deactivation by blocking the ligand (“PD-L1”) of T cell protein PD-1. Because ICIs enhance intrinsic immune defenses, their most important side effects are “immune related adverse events” (irAE).
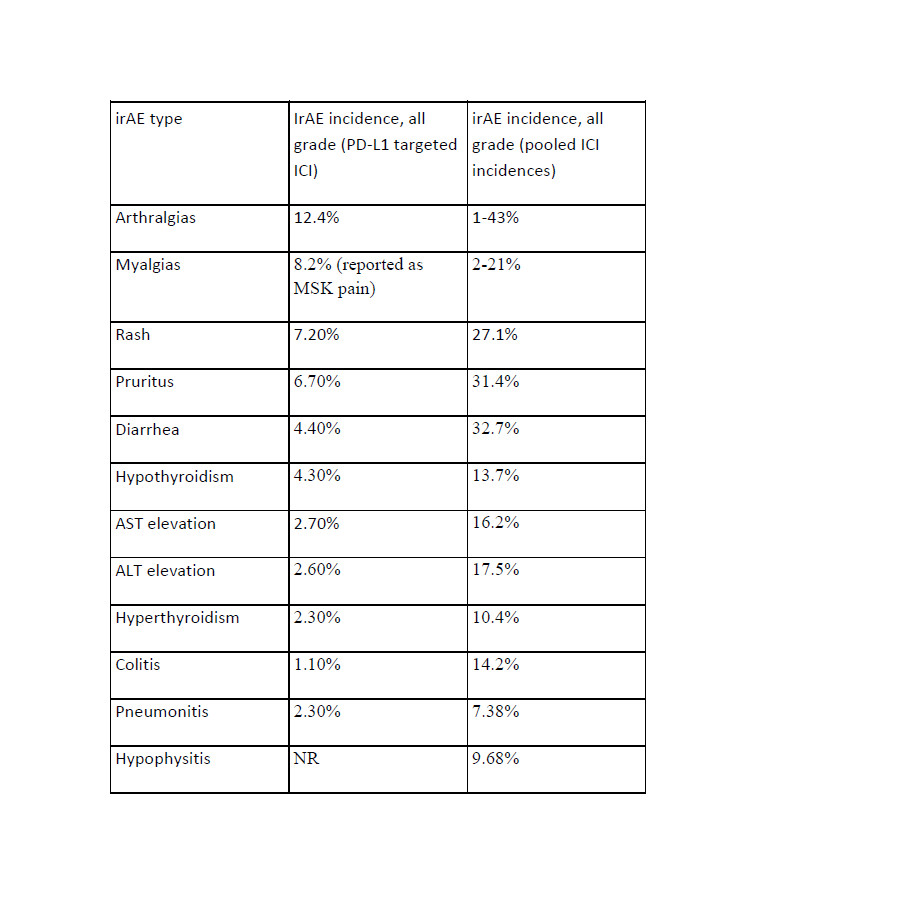
PD-L1 inhibitors seem to have lower irAE rates compared with other forms of ICI therapy.1,2
The most common reported irAEs involve the GI tract, endocrine system, skin and liver.3 Previously reported rheumatic irAEs have included rheumatoid arthritis, polymyalgia rheumatica, psoriatic arthritis, GCA, arthritis, myalgias, and arthralgias4. Inflammatory arthritis is a comparatively infrequent irAE5.
In one case series, 50% of patients who required either glucocorticoids or a delay in treatment with PD-1 or PD-L1 inhibitors had no further irAEs after re-initiation of ICI therapy.3 Of patients who did have a flare, 24% had a recurrence of the initial event, while 26% experienced a new irAE.3
This patient’s resolution without recurrence after a short course of steroids suggests that a brief trial of low dose steroid is a reasonable treatment plan for patients with oligoarthritis as an irAE after ICI.
Of note, in subsequent weeks the patient developed radiation pneumonitis, known to be statistically associated with Durvalumab therapy.4
Conclusions: Immunotherapies for cancer are becoming more widely used. Hospitalists and primary care physicians should be on the lookout for immune related adverse events in patients on these medications.