Background: As hospitalists take over additional patient care duties in teaching hospitals, many issues that impact residents are now being experienced by hospitalists. Previous studies have shown that between 22% and 27.7% of nighttime pages were nonurgent, including patient-status updates, low-priority order request, and non-critical lab values. Unnecessary interruptions distract from patient care, contribute to burnout, and decrease physician-nurse collaboration. Additionally, as hospitalists we often experience circumstances that make our work more difficult that we feel powerless to change. We present a hospitalist-led quality improvement (QI) project aimed at reducing unnecessary nighttime pages at a public safety-net teaching hospital.
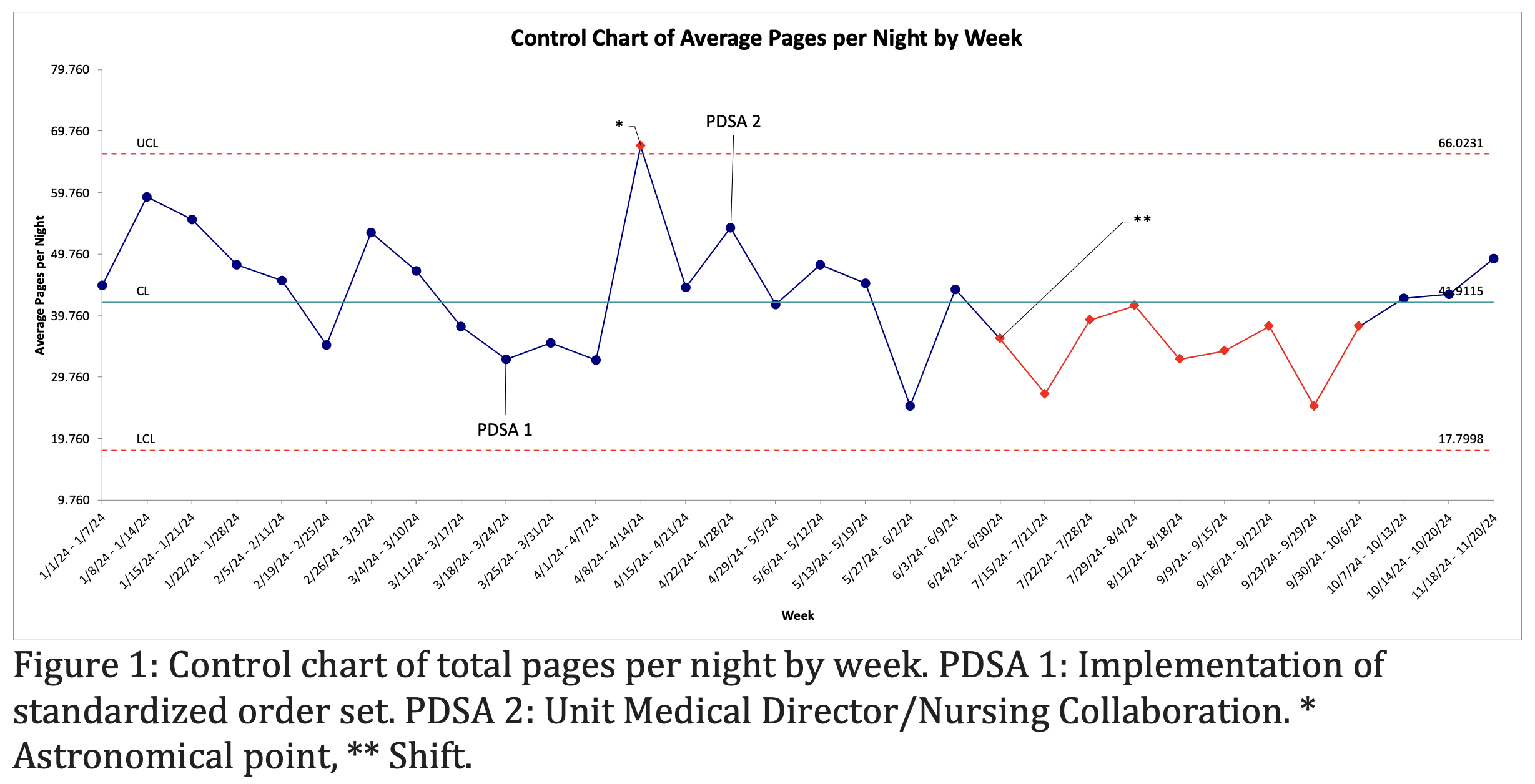
Methods: At the end of each overnight shift, the on-call hospitalist documented key metrics in a shared Microsoft Excel file, including the total number of pages, the number of admissions, and the patient census at the start of the shift. These data were reviewed during monthly meetings, where the data collection tool and metrics were refined based on team feedback. Using Plan-Do-Study-Act (PDSA) methodology, iterative cycles were conducted with ongoing review of measures to guide improvement efforts. Data were grouped by week and visualized using control charts. All analyses were performed using Microsoft Excel (Version 16.91) and QI Macros for Excel (Version 2021.07).
Results: Our project began on November 15, 2023, with an initial focus on refining data collection methods. From January 3, 2024, to March 18, 2024, we collected data to establish a baseline, with an average of 46.9 total pages per night. The first PDSA cycle implemented a standardized order set, incorporating modified vital sign notification parameters and PRN medications for pain, nausea, and sleep. The second PDSA cycle involved collaboration between hospitalists serving as unit medical directors and nurses to identify and defer non-urgent nighttime pages—such as restraint renewals, updates to isolation status, and documenting medical necessity for urinary catheters—to the morning. Our results are presented as a control chart (Figure 1). A significant astronomical point was observed in the week of April 8. During this week, a hospitalist was on nights that had not implemented the standardized order set and experienced an unusually high number of admissions. Following this week, the hospitalist implemented the standardized order set. Between July 24 and October 6, a significant downward shift in was noted. Over the period from July 15 to November 19, the total pages per night averaged 38.5—a reduction of 18% compared to the baseline.
Conclusions: Our project shows how a hospitalist-led QI project can result in decreases in total pages at night. Additionally, this project demonstrates how a QI initiative can engage and empower hospitalists to be agents of change. Our group was initially challenged with obtaining data. Through the implementation of an easy collection instrument that our hospitalists could directly enter data into, enough data was collected to conduct our project. Our primary intervention focused on elements of the process that were within the control of our hospitalist (eg: standardized order set). Another result was increased collaboration between our hospitalist attendings and nurses. The combination of these two simple interventions resulted in an 18% reduction in nighttime pages. Our project serves as a model for a hospitalist-led initiative that can reduce nighttime pages.