Background: TeamSTEPPS (Strategies and Tools to Enhance Performance and Patient Safety) has been shown to improve patient safety by improving teamwork and communication skills amongst all members of the interdisciplinary team.
Methods:
We developed a 4-hour TeamSTEPPS multi-disciplinary training session, conducted in our simulation center. We invited 90 core members of the medicine service to participate. Participants represented the following 5 disciplines: hospitalists, nurses, care managers, social workers, and trainees/nurse practitioners/physician assistants. We trained 15 participants each session (3 participants per discipline). We held 6 identical sessions over a 4 month period.
Each session consisted of a short didactic session on patient safety and TeamSTEPPS training delivered by department of medicine leadership.
Participants were divided into three groups, each consisting of a hospitalist, a nurse, a care manager, a social worker and a trainee/NP/PA. Each group rotated through three different scenarios that were devised to mimic real-life: interdisciplinary rounds, a team huddle and an end-of-life discussion with a standardized patient at the bedside. Each participant was given some but not all of the relevant information and asked to play his or her own role (so a social worker would play a social worker) in the scenarios. A facilitator gave feedback and taught one of three TeamSTEPPS strategies for improved communication: CUS (concerned/uncomfortable/stop for safety), SBAR (situation, background, assessment, recommendation) or check back. For the final session, participants were introduced to and practiced IPASS as a method of signout.
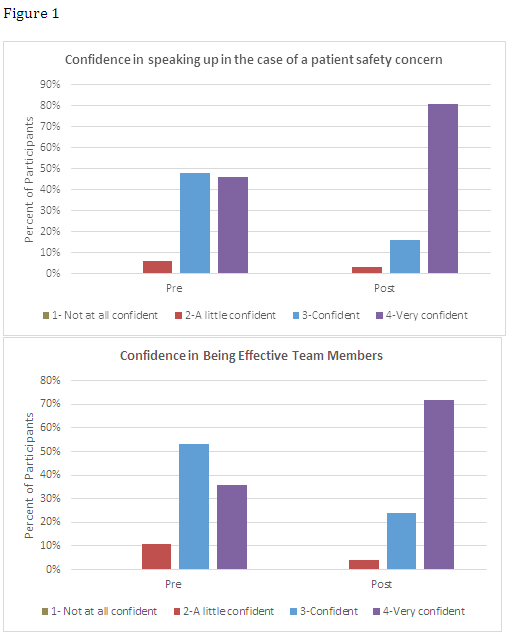
Change in participant’s skill confidence was assessed after each workshop using a retrospective pre post survey using a 4 point scale from “not confident” to “very confident”. Participants completed commitment to change (CTC) statements after each workshop. The primary outcome was a comparison of participants’ comfort levels with a.) being an effective team member and b.) speaking-up before and after training as determined by a survey (filled out anonymously by participants before leaving the session). The secondary outcome was the percentage of participants who fulfilled their CTC after at least one month.
Results:
87 health-care professionals participated in the TeamSTEPPS training session.
76% would “definitely” and 20% would “probably” recommend the session to a colleague.
Participant confidence, as measured by the retrospective pre-post assessments, improved in the ability to be an effective team member from 36% to 72% “very confident” and in the ability to speak up in the case of a patient safety concern from 46% to 81% “very confident” (Figure 1).
Of the 87 participants, 32 reported back on their CTC after at least 1 month. Of these, 88% fulfilled their commitment.
Conclusions:
TeamSTEPPS training helped participants feel more comfortable in being effective team members and in speaking up.