Case Presentation:
A 62 years old male presented to the emergency department with soft tissue swelling, urticarial skin rash and acute respiratory failure. He was diagnosed with acute anaphylactic reaction with angioedema. He was given IV Epinephrine, Benadryl and solumedrol. Shortly he was intubated for airway protection.
Although the Initial EKG was unremarkable, shortly the cardiac monitor displayed inferior leads ST segment changes, repeat EKG showed ST elevation in inferior leads (II, III and AVF).
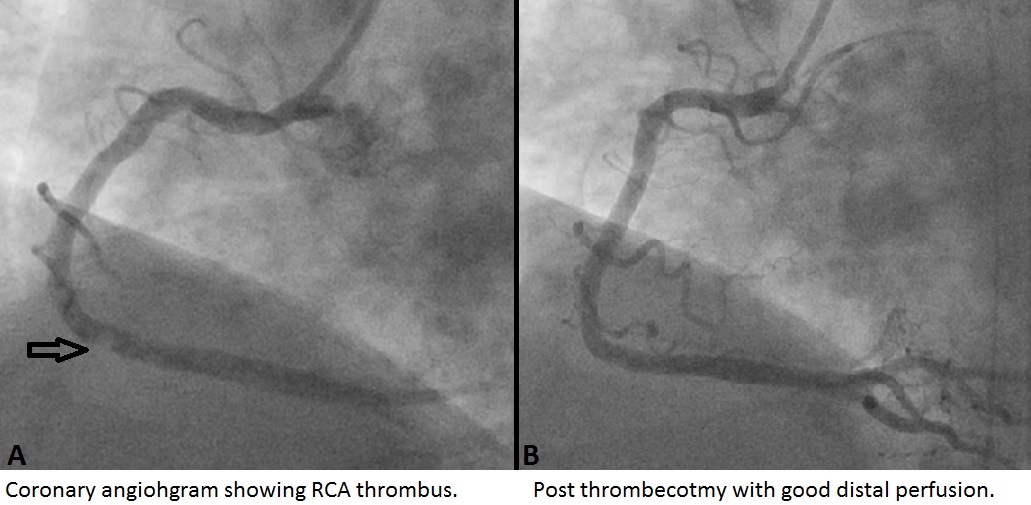
The patient was rushed to the Cath-lab, coronary angiogram revealed a thrombus in mid right coronary artery without underlying plaque lesion. The thrombus was suctioned with a thrombectomy catheter, neither coronary balloons nor stents were used. His only other angiographic finding was 30% stenosis of mid LAD artery.
Later he reported history of allergic reactions to unknown allergen for which he was prescribed an Epi pen. He was discharged on dual antiplatelet therapy.
Discussion:
Anaphylaxis is a systemic reaction with multisystem involvement, including skin, airway, vascular and gastrointestinal systems. Anaphylaxis can rarely trigger coronary spasm and ST myocardial infarction even in patients without underlying coronary artery disease, which is known as Kounis syndrome (KS).
Two major variants of KS were described; Type I variant includes patients with normal coronary arteries in whom the acute allergic reaction induces coronary artery spasm with or without infarction. Type II variant includes patients with pre-existing atheromatous disease in whom acute allergic episode can induce plaque erosion or rupture manifesting as an acute myocardial infarction. Recently other variants were described such as anaphylaxis triggering late thrombosis in a drug eluting stent, and KS in a coronary bypass graft.
Many allergens reported to induce KS including antibiotics, analgesics, antineoplastic, contrast media, anesthetics, thrombolytic and NSAID’s.
The pathophysiology of KS is amplified degranulation of mast cells. In the heart, mast cells have perivascular distribution close to myocyte and arterial intima. During their degranulation, several vasoactive compounds (histamine, prostaglandin-D2, thromboxane, and leukotrienes) and collagen-degrading compounds are released locally and in the peripheral circulation, causing coronary vasoconstriction. Additionally, histamine-mediated endothelial activation can cause coronary artery spasm and plaque rupture. Histamine also activates platelets, triggering thrombosis. Genetics might play role in determining predisposition to KS.
Coronary intervention is the best approach to diagnose and treat coronary occlusions in KS presenting with STEMI.
Conclusions:
Kounis syndrome should be considered in patients presenting with acute coronary syndromes in the context of acute anaphylaxis. Coronary intervention is the best approach for management. Further research is required to establish preventive and interventional measures.