Background: During 2016, the total billed cost of cardiac monitoring neared 4 million dollars at our institution and many patients were observed on the monitor without approved indication as published by the American Heart Association’s (AHA) guidelines published in 2014. The overutilization of cardiac monitoring constitutes a misappropriation of resources which results in undue health care cost.
Purpose: This project aimed to reduce total telemetry cost by 15% or decrease telemetry related costs by 1 million dollars yearly without increasing RRT/code events by March 2018.
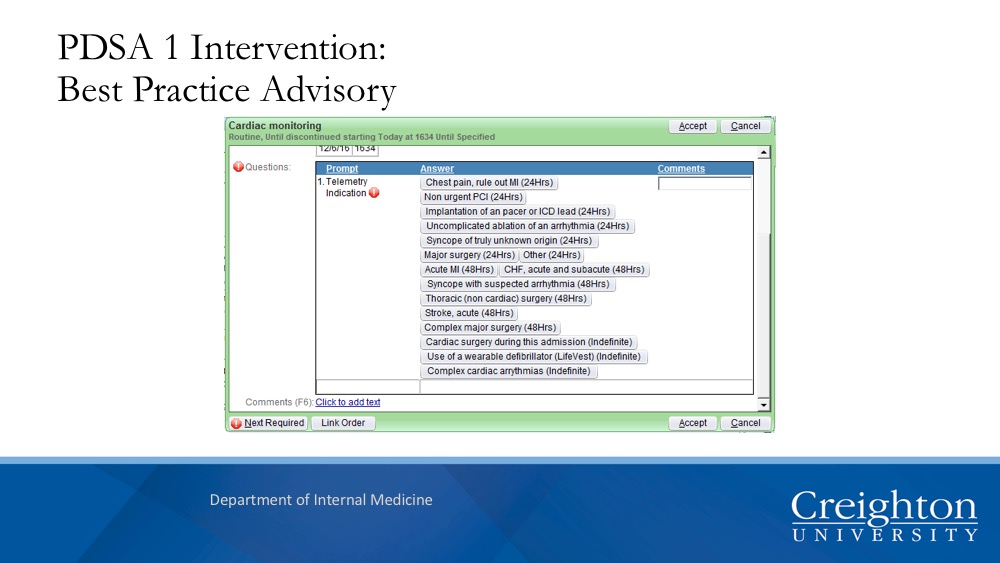
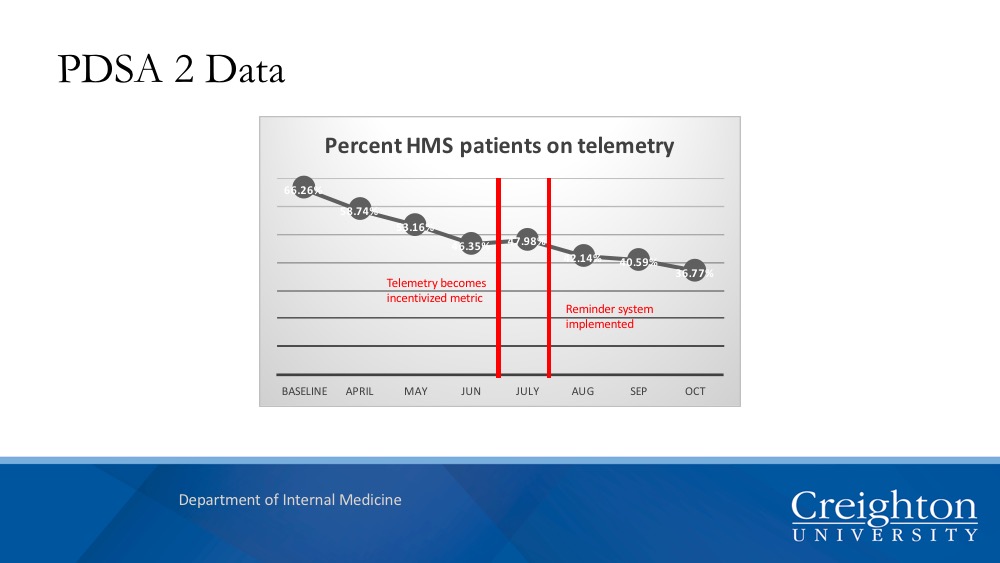
Description: Using the Plan-Do-Study-Act (PDSA) methodology, the team used baseline telemetry metrics to develop interventions that were implemented in two successive PDSA iterations. Telemetry census and Code/RRT data were collected in tandem for inpatients between October 2016 and November 2017. In PDSA1, a Best Practice Advisory (BPA) prompted providers to select AHA approved indications for cardiac monitoring. In PDSA2, telemetry reduction became an incentivized metric for hospital medicine staff and a reminder system was implemented to make providers aware of which patients were on telemetry.
Telemetry census data compiled from PDSA1 showed that after application of the BPA, there was a 2% reduction in monitored patients in unit 5200 and a 5% reduction in patients monitored in units 5400/5500. Code blue rates decreased from 9.147 per 1000 discharges to 9.02 per 1000 discharges. The rapid response rate increased slightly from 15.944 to 16.64 per 1000 discharges. In PDSA2, a 9.6% decline in cardiac monitoring was observed. The code blue rate declined slightly from 6.87 to 6.34 per 1000 discharges and the rapid response rate declined from 72.33 to 59.58 per 1000 discharges.
Conclusions: Each iteration of PDSA has resulted in a measurable decreased in cardiac monitoring without a significant increase in codes or RRT events. These data represent a possible translatable model for other medical centers.