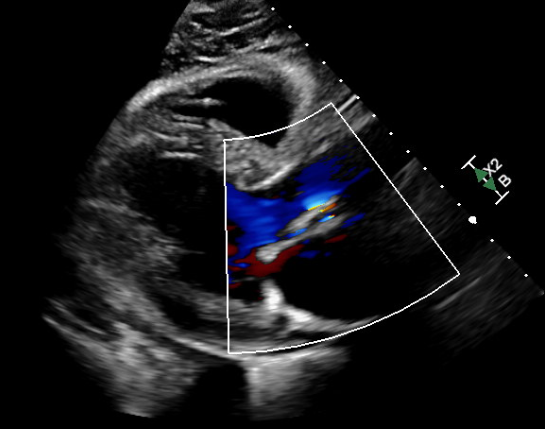
Case Presentation: History: A 67-year-old male with a complex medical history, including HIV on HAART, Type 2 diabetes mellitus (T2DM), stage III CKD with microalbuminuria, severe aortic stenosis treated with TAVR, and post-procedural complete heart block managed with a dual-chamber pacemaker, presented to the emergency department with right-sided abdominal pain. This pain, described as cramping, mild to moderate in intensity, began shortly after routine outpatient lab results showed significantly elevated LFTs and LDH. His TAVR procedure, performed a month earlier, was uneventful except for the need for permanent pacemaker placement due to complete heart block.Clinical Findings: On presentation, vital signs were stable. Physical examination revealed a regular heart rhythm, grade II/VI systolic murmur at the right sternal border, and no peripheral edema. Initial laboratory workup was notable for hemoglobin of 10.9 g/dL, elevated total bilirubin (2.8 mg/dL), normal direct bilirubin (0.3 mg/dL), AST of 67 U/L, and LDH of 792 U/L, with a marked reduction in haptoglobin (< 10 mg/dL). Renal function was stable with a creatinine level of 1.23 mg/dL. Imaging, including a CT of the abdomen and pelvis, showed no acute abnormalities.Echocardiography Findings: Follow-up echocardiography revealed a well-seated 26-mm Edwards bioprosthetic valve with a mean gradient of 13 mmHg, an aortic effective orifice area of 1.4 cm², and mild-to-moderate aortic periprosthetic leak. Left ventricular systolic function remained preserved (LVEF 55-60%).Hospital Course: Hematology and infectious disease consultations were sought. Given the elevated LDH, decreased haptoglobin, and evidence of a paravalvular leak, hemolytic anemia secondary to mechanical trauma from the TAVR prosthesis was suspected. The patient’s total bilirubin decreased to 1.4 mg/dL with supportive care. Close monitoring of hemoglobin levels was recommended, with outpatient follow-up planned.
Discussion: TAVR is a transformative procedure for severe aortic stenosis, offering an alternative to surgical valve replacement for high-risk patients. However, it is not without complications. Hemolytic anemia, though rare, is a recognized adverse event often associated with paravalvular leaks or high prosthetic valve gradients.The mechanism of hemolysis in this patient likely involved mechanical shearing forces and turbulent flow caused by the mild-to-moderate paravalvular leak. This leak was confirmed on echocardiography, with a decreased aortic effective orifice area and elevated LDH levels supporting hemolysis as the primary etiology.Diagnostic Considerations: The differential diagnosis included infection-related anemia secondary to HIV, hepatobiliary pathology, and drug-induced hemolysis from HAART. However, the rapid onset of symptoms post-TAVR and the absence of infection or hepatobiliary abnormalities directed the focus to mechanical hemolysis.Management Strategies: Mild cases of hemolysis can be managed conservatively with close monitoring, as in this patient. Severe cases may require percutaneous or surgical interventions to correct the paravalvular leak. Advances in TAVR prosthesis design and procedural techniques aim to minimize such complications.
Conclusions: Paravalvular leaks, though often mild, can result in significant mechanical hemolysis, leading to anemia and other systemic effects. Early detection and intervention are critical to addressing paravalvular leaks and mitigating their impact on patient health.