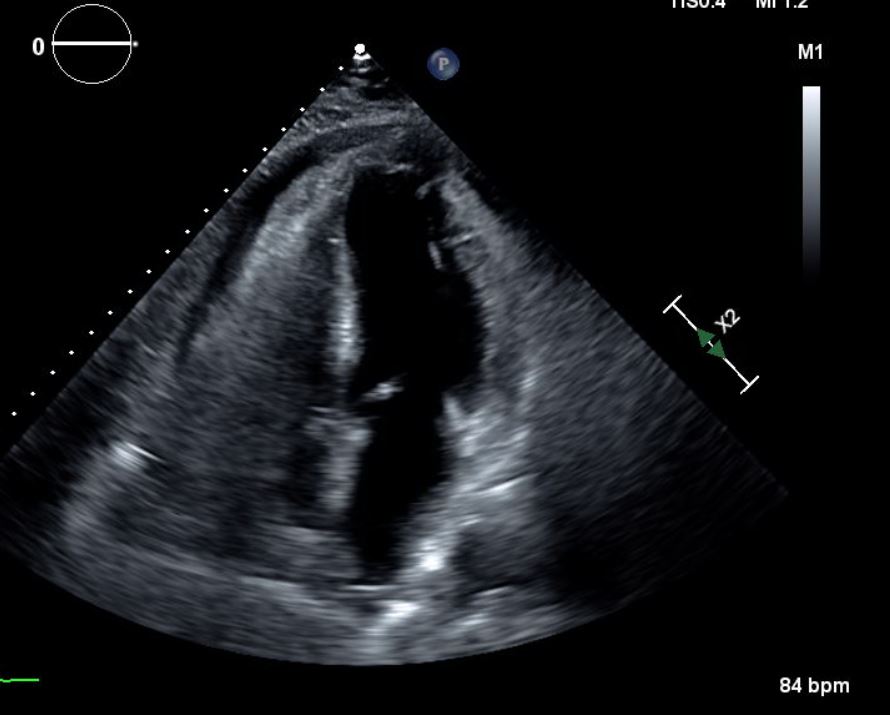
Case Presentation: A 77-year-old caucasian man with a known history of hypertension, hyperlipidemia and tobacco abuse initially presented to the hospital with chest pain for five days. He was diagnosed with an anterior wall ST elevation myocardial infarction (STEMI). He underwent cardiac catheterization with drug-eluting stent placement to the left anterior descending coronary artery. Subsequent transthoracic echocardiogram (TTE) showed a left ventricular ejection fraction of 45%, and a large left ventricular (LV) thrombus. The patient was anticoagulated, medically optimized and discharged home. He returned one month later with recurrent chest pain prompting a repeat TTE, which demonstrated resolution of the LV thrombus with a new pericardial effusion and pseudoaneurysm. The patient underwent urgent cardiothoracic surgery with patching of the LV rupture with pericardium and his immediate postoperative course was uncomplicated. A repeat TTE immediately post-op revealed no LV thrombus. He was discharged home not on anticoagulation. Follow up TTE 3 weeks later demonstrated recurrent LV thrombus. Follow up TTE at 6 weeks demonstrated resolution of LV thrombus with residual LV apical dyskinesis and no pericardial effusion.
Discussion: LV pseudoaneurysm is a rare, but serious complication of acute myocardial infarction that occurs more commonly with late presentation of STEMIs. Due to modern medical management and prompt attention to STEMIs, this phenomena occurs only in approximately 0.3% of patients who have suffered an MI. Despite its low incidence, it should remain high on the differential diagnosis for patients presenting with chest pain or dyspnea after a MI, due to its high mortality rate. A timely and accurate diagnosis is the difference between life and death for the patient. Untreated cases have a 30-45% risk of complete rupture; medical management alone carries a near 50% mortality. TTE remains the mainstay for diagnosis, with echo contrast available to assist in visualization. Once a diagnosis is definitively made, urgent surgical repair is indicated as definitive, often lifesaving therapy.
Conclusions: Given its life threatening nature, a cardiac pseudoaneurysm must be identified and corrected rapidly. It typically occurs 3-5 days post myocardial infarction and the index of suspicion must be high in patients with the appropriate clinical history. Due to modern interventions, patients spend more of their recovery time on the general medial floor under the care of a hospitalist, highlighting the need for awareness of such a condition. Being alert and acting quickly with regards to a pseudoaneurysm can save a life.