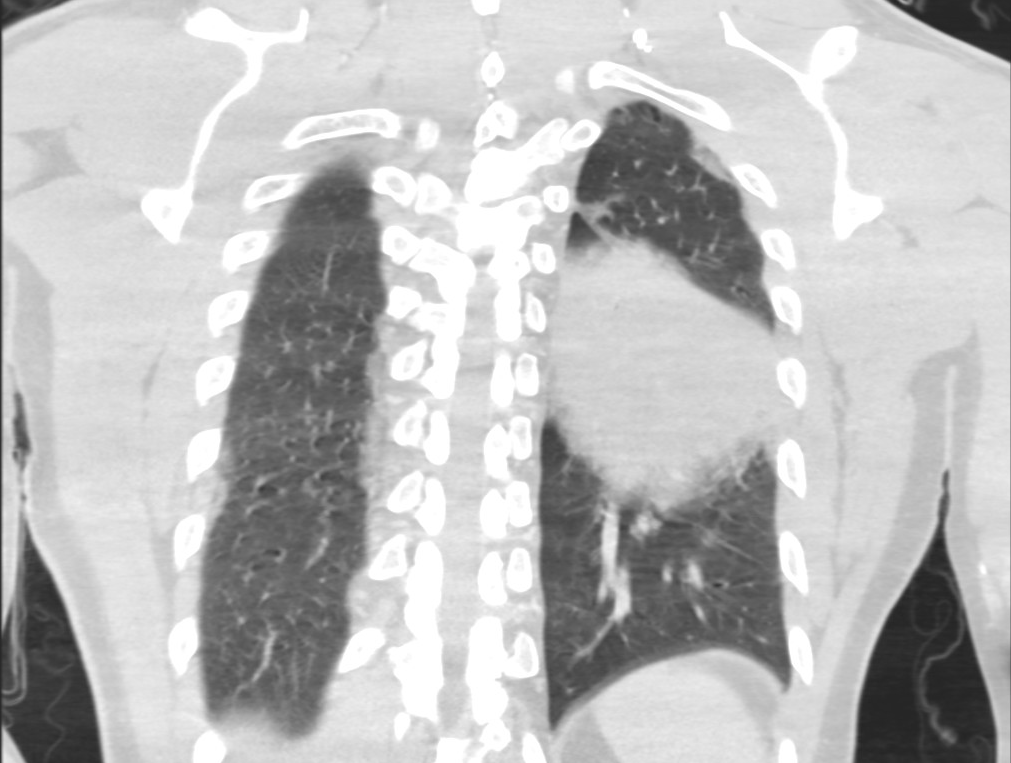
Case Presentation: A 43-year-old man with ankylosing spondylitis (on adalimumab), presented with 2-days of fever, cough, diarrhea, and encephalopathy. He had no significant travel history. On exam, he was tachycardic (P = 120 bpm), febrile (temperature 103.0oF), tachypneic (RR = 30 bpm) and had left-sided crackles. Notable labs: WBC = 12.3 109/L, Na+ = 130 mmol/L, creatinine = 1.75 mg/dL; lactate and transaminases were mildly elevated. CT angiogram of the chest showed consolidation in the superior segment of the left lower lobe and patchy ground glass infiltrates in the left upper lobe. He was initially treated with ceftriaxone and azithromycin. Sputum and blood cultures were negative. He deteriorated despite antibiotics; his clinical course was complicated by acute hypoxic respiratory failure requiring intubation, acute kidney injury requiring hemodialysis, shock requiring pressors, and rhabdomyolysis. He was negative for HIV and mycobacterium tuberculosis. Urine antigen and tracheal aspirate were positive for Legionella pneumophila serotype 1 antigen. He was transitioned to monotherapy with azithromycin but remained febrile; 8 days later, azithromycin was stopped and levofloxacin was started. His fevers briskly subsided and clinical improvement was noted.
Discussion: Legionnaire’s disease remains on the differential for community-acquired pneumonia. Since its discovery over 50 years ago, incidence rates of Legionella pneumonia have risen partly due to improved diagnostics and increased awareness [1]. The index of suspicion is increased in patients with pneumonia who also present with gastrointestinal symptoms, hyponatremia, and elevated transaminases, particularly if immunocompromised. Our case highlights the use of anti-tumor necrosis factor (TNF)-α antagonist as an important risk factor for legionellosis and severe infection. An associated risk of legionellosis with anti-TNF-α treatment was described in a prospective study of French registry data on 10 patients, with the associated relative risk estimated between 16.5 and 21.0 [2]. Additional studies have demonstrated that the risk of severe infection is higher in those receiving anti-TNF-α immunotherapy [4-6]. Another notable feature of this case is the patient’s lack of clinical response prior to being transitioned from a macrolide to a fluoroquinolone. Recent meta-analyses from 2014 and 2021 demonstrated no significant difference in mortality outcomes between the use of the two agents, although both showed a trend towards lower mortality with fluoroquinolones [7-8].
Conclusions: A history of anti-TNF-α immunotherapy is an important risk factor for legionellosis and progression to severe disease. While the current guidelines suggest that either macrolides or fluoroquinolones are adequate as monotherapy, our case highlights the need to consider fluoroquinolones over macrolides in immunocompromised patients with severe Legionnaire’s disease.