Background: Diagnostic and clinical reasoning errors are common and a source of harm to our patients. Improving clinical reasoning skills is challenging due to the absence of feedback. Care transitions have been recognized as an area of vulnerability for hospitalized patients, however, they also represent opportunities for error recognition and improvement as the oncoming clinician reviews and revises the established diagnoses. We sought to leverage care transitions to provide an opportunity for a review of diagnoses and to quantify the rate and types of diagnostic errors in hospital medicine.
Methods: We used a questionnaire to identify diagnostic changes and describe whether changes were due to diagnostic change, disease evolution or diagnostic refinement.1 We created a report to identify patients admitted from Thursday-Saturday to the hospital medicine services and transitioned from one hospitalist to another at end of the service week. The hospitalist assuming care was assigned up to 2 patients meeting study criteria to describe whether diagnostic change occurred. This process started in April 2019 until March 2020 and from May 2020 until August 2021.Completed questionnaires with a diagnostic change were then independently reviewed by two physician team members using the Revised SaferDx Instrument.2 If there was disagreement between the two reviewers on whether an error occurred, a third reviewer adjudicated disagreements. All reviewers were blinded to each other’s reviews and recused themselves if involved in the case. Using these reviews, we established the rate of diagnostic change and diagnostic errors along with the type of harm that occurred from the errors. We then provided written feedback to hospitalists about their cases in which there were diagnostic changes both with and without errors. The feedback forms were emailed to the hospitalists prior to a meeting with a study team member to discuss their feedback, ask questions, and review findings. We solicited feedback from hospitalists on the survey and feedback process.
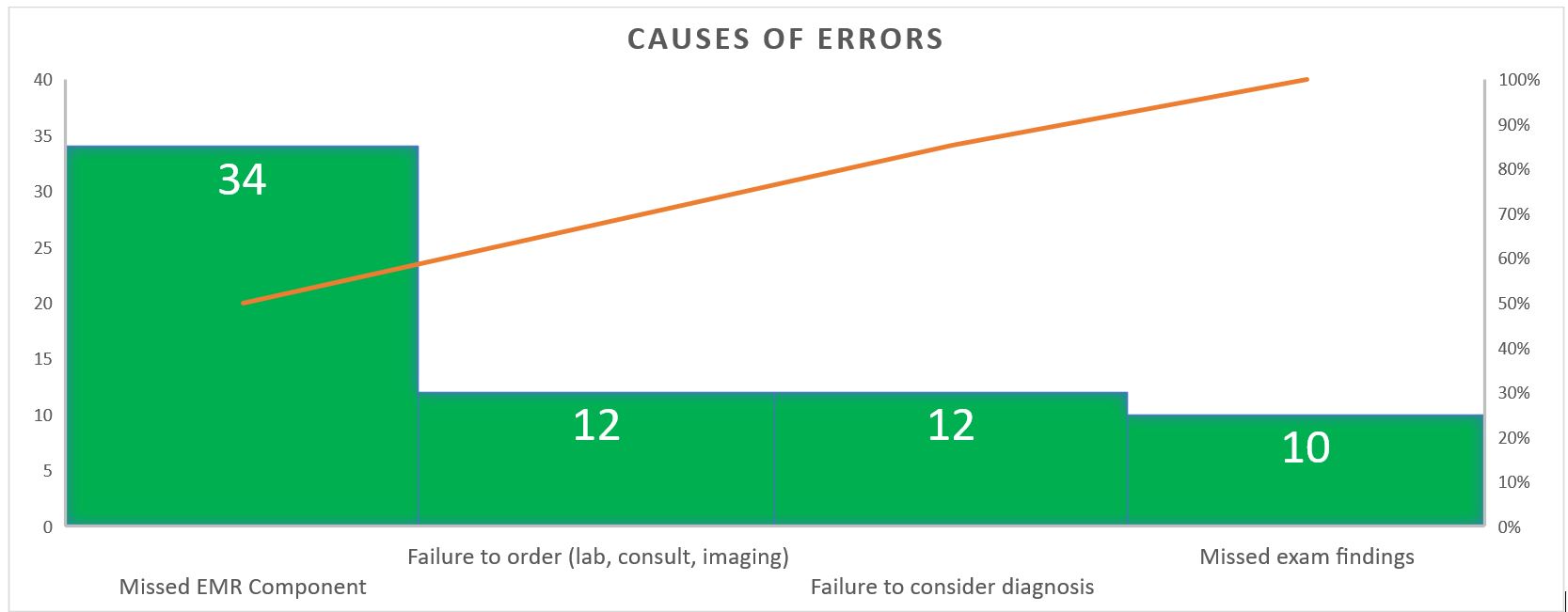
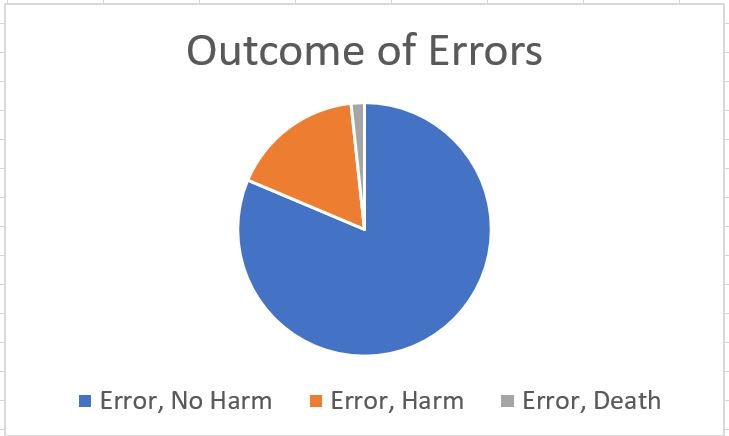
Results: Overall, 621 of 641 questionnaires were completed for a 97% response rate. 184 out of 1011 total patients (18.2%) had a diagnostic change. After adjudication, 59 of 1011 patients (5.8%) in our study sample were found to have a diagnostic error. The team then reviewed errors and identified four main causes of errors (Figure 1): 1) Missed components in the electronic health record (EHR) 2) Failure to consider diagnosis 3) Failure to order a test or consult 4) Missed physical exam findings. We next identified the type of harm which occurred (Figure 2) and 48 of 59 error cases (81.4%) did not cause harm, 10 of 59 cases (16.9%) caused some harm and 1 case of 59 had an error that likely contributed to death. Hospitalists received the feedback reports positively and found it beneficial to learn about errors.
Conclusions: Our study shows hospitalist care transitions can be used to identify and categorize diagnostic errors. Our experience also finds hospitalists are open to feedback on diagnosis and clinical reasoning. Some reported the study encouraged them to preemptively notify colleagues about diagnostic changes or errors which improves the culture of feedback overall in our group. This study provided valuable information on the types and causes of errors however our method required manual chart reviews and adjudication which was labor-intensive. We plan to further study this process in the emergency department and with internal medicine residents.