Background: The US healthcare system is under increasing pressure to improve value and affordability. Acute care is responsible for a large proportion of overall health costs, but the complexities and pace in this environment have left an evidence gap in value-based care transformation. Novel improvement and evaluation strategies are thus needed more than ever to guide such efforts. The combination of Lean manufacturing methodology with the rigor of applied research may create a powerful, conceptual framework to guide the generation of real-world evidence in acute care value.
Purpose: This case study outlines the approach we used to leverage Lean methods to rapidly design and test the feasibility of a standardized care pathway as preparation for an applied research study, called the AECOPD Pathways Trial (Acute Exacerbation of Chronic Obstructive Pulmonary Disease).
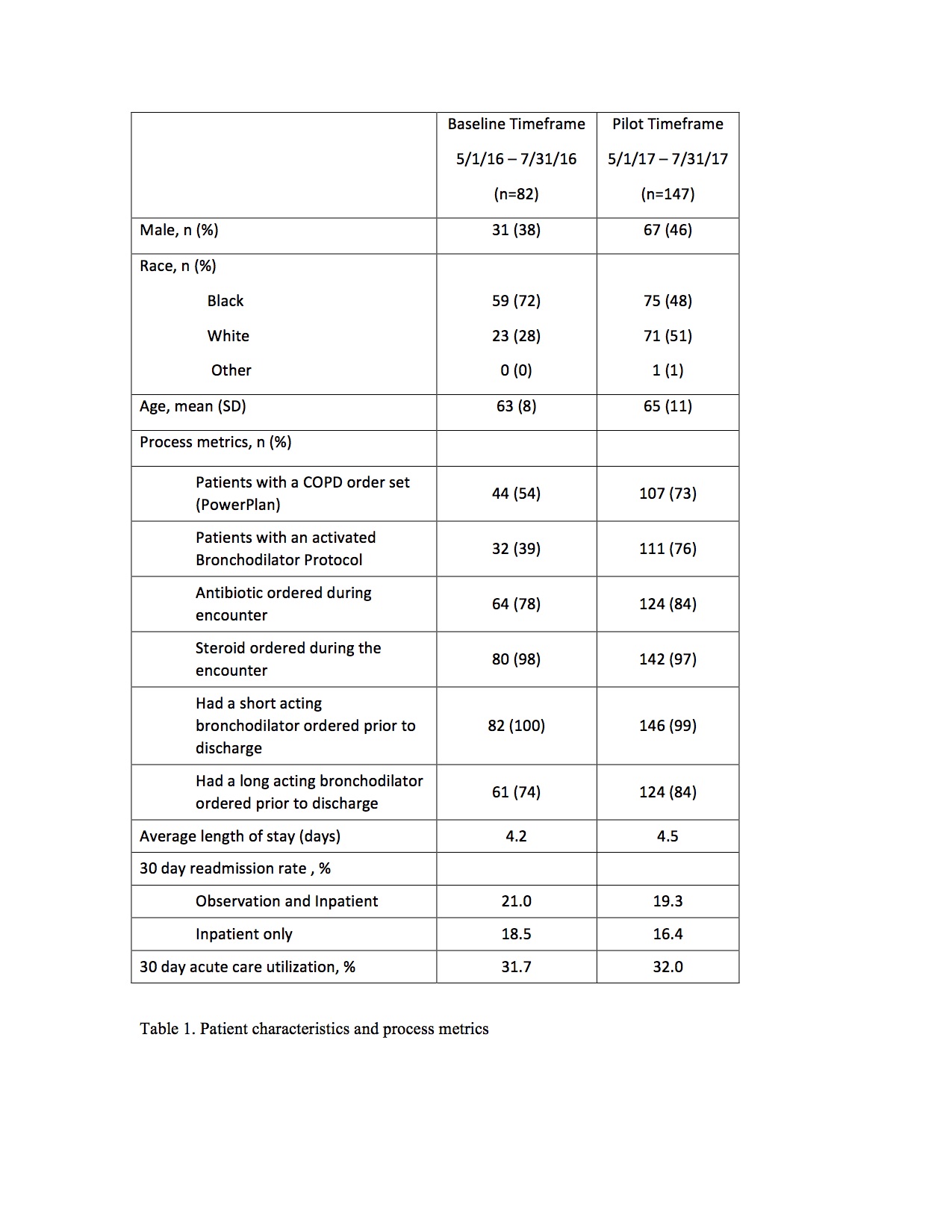
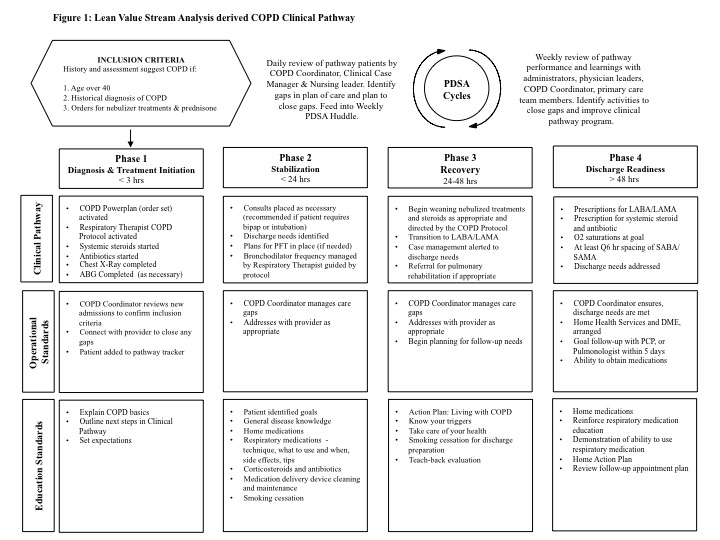
Description: The AECOPD Pathways Trial aimed to compare the effectiveness of the care pathway versus usual care on utilization outcomes. At a single hospital site, the Lean and research teams: (1) defined the current state of care processes for patients admitted with AECOPD; (2) engaged stakeholders across the care continuum; and (3) piloted the implementation of a comprehensive COPD care pathway. Using the Lean Value Stream Mapping (VSM) approach, guided by chart reviews, the components of AECOPD inpatient care were categorized into 4 phases with corresponding activities: (a) Diagnosis and treatment initiation; (b) Stabilization; (c) Recovery; and (d) Discharge readiness (Figure 1). The pilot commenced May 2017 with daily and weekly huddles to inform improvements made through Plan, Do, Study, Act (PDSA) cycles. Metrics are compared from May-July 2016 (Pre-Pilot) and May-July 2017 (Pilot). Patients were included in the analyses if they were over 40 years old and had a discharge diagnosis of COPD exacerbation (ICD10 code 44.1).In the Pre-Pilot period, 82 patients met inclusion compared to 147 in the Pilot period. The 2017 cohort had higher percentages of Caucasian and male patients. Utilization of the COPD order set and bronchodilator protocol (both key components of the care pathway) increased from 54% and 39% in 2016 to 73% and 76% in 2017 respectively. Long acting bronchodilator orders placed prior to discharge increased from 74% in 2016 to 84% in 2017. Other process measures were similar across time periods. These process measures and outcomes metrics are reported in Table 1. The finalized care pathway created in this Lean/Applied Research pilot is now successfully being implemented at 8 hospitals in the COPD Pathways Trial.
Conclusions: This quality improvement pilot demonstrates the approach of leveraging Lean methodology to inform the design of an applied research study intervention. The combined approach resulted in synergies that neither method could accomplish alone improving the protocol’s alignment with stakeholder needs and acute care workflows. Learning health systems can use this framework to enable effective and efficient generation of value-based evidence in real-world, acute care settings.