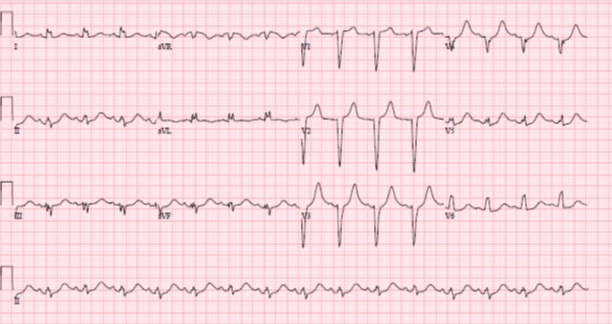
Case Presentation: The patient is a 13-year-old female with attention-deficit/hyperactivity disorder (ADHD) and depression who presented following an intentional overdose of her lisdexamfetamine (Vyvanse™). She admitted to taking 15 – 40mg tablets in addition to 5 tablets of an unknown, over the counter sleep aid. She developed dizziness and mild non-radiating substernal chest pressure 10-15 minutes after ingestion. In the ED, her chest pain resolved but she had hypertension with significant orthostatic tachycardia. Serial ECGs revealed left axis deviation and borderline prolonged QTc with no pathologic ST segment changes (image 1). Upon standing, approximately 14 hours after ingestion, she developed wide complex tachycardia and dizziness followed by syncope. Her troponin T was markedly elevated at 0.64 ng/mL (normal <0.09ng/mL). A transthoracic echocardiogram showed regional wall motion abnormality of the interventricular septum and normal coronary artery origins. She was treated with aspirin and intravenous esmolol infusion in the context of worsening tachycardia and hypotension. 20 hours post ingestion she developed a persistent left bundle branch block (LBBB) (image 2). Her LBBB resolved at approximately 96 hours post ingestion and the esmolol was stopped. Her cardiac biomarkers and ventricular function normalized by 7 days after ingestion and she was discharged to inpatient psychiatric facility.
Discussion: Lisdexamfetamine is a commonly used psychostimulant used for the treatment of ADHD. It stimulates the central nervous system via release of dopamine, norepinephrine, and serotonin. These neurotransmitters also act on other organ systems including the heart and are well known to lead to vasoconstriction, tachycardia and have the potential to cause myocardial ischemia. Lisdexamfetamine overdose has previously been associated with QTc prolongation and hypertension. Case series describe amphetamines causing biphasic heart rate response, coronary vasospasm and left ventricular dysfunction. However, in our review of the literature there is only a single case of Lisdexamfetamine induced coronary vasospasm in an adult.
Myocardial ischemia in adults is most commonly caused by atherosclerotic disease leading to thrombosis but this etiology is extremely uncommon in pediatric patients. Typically when children present with classic ST elevations in a typical distribution on ECG and a presumed diagnosis of myocardial ischemia is made the most likely etiologies are conditions that cause coronary artery inflammation (e.g. Kawasaki Disease) or anatomic abnormalities like anomalous coronary arteries. Other conditions to consider include coronary vasospasm which was the presumed diagnosis in this patient given the rapid improvement in symptoms without intervention. This patient did not have classic ST segment elevations or persistent chest pain which made the diagnosis more challenging. Eventually she developed LBBB which combined with wall motion abnormality seen on echocardiogram confirmed the diagnosis of myocardial ischemia. She did not undergo cardiac catheterization, despite being the gold standard test for diagnosis of coronary vasospasm because her ECG changes were late to develop and her chest pain had resolved.
Conclusions: Given the regular use of lisdexamfetamine in the pediatric population hospitalists should be aware of the potential for myocardial ischemia in patients admitted with overdose, even in those who don’t immediately present with classic signs and symptoms.