Background: Cardiac arrest, as characterized by an abrupt loss of cardiac function, remains to be a main event preceding death with low survival rates nationwide. Although many factors can serve as the underlying etiology, it is agreed upon that prompt response with the initiation of advanced cardiac life support is the cornerstone of preventing mortality. In this study we focus on the increasing incidence of cardiac arrest nationwide. Furthermore, we highlight the difference in rates of survivability in patients who experienced cardiac arrest in teaching hospitals versus non-teaching hospitals.
Methods: We surveyed Healthcare Cost and Utilization Project (HCUP) Hospital Inpatient National Statistics from years 1997 to 2014 in the United States to identify patients with cardiac arrest and ventricular fibrillation using the Clinical Classification Software (CCS). Total incidence and mortality from cardiac arrest and ventricular fibrillation were obtained in both urban teaching and urban non-teaching hospitals. Additionally, number and percent in-hospital deaths were compared between teaching and non-teaching hospitals. Z-test was used to obtain a two-tail p-value to determine statistical difference.
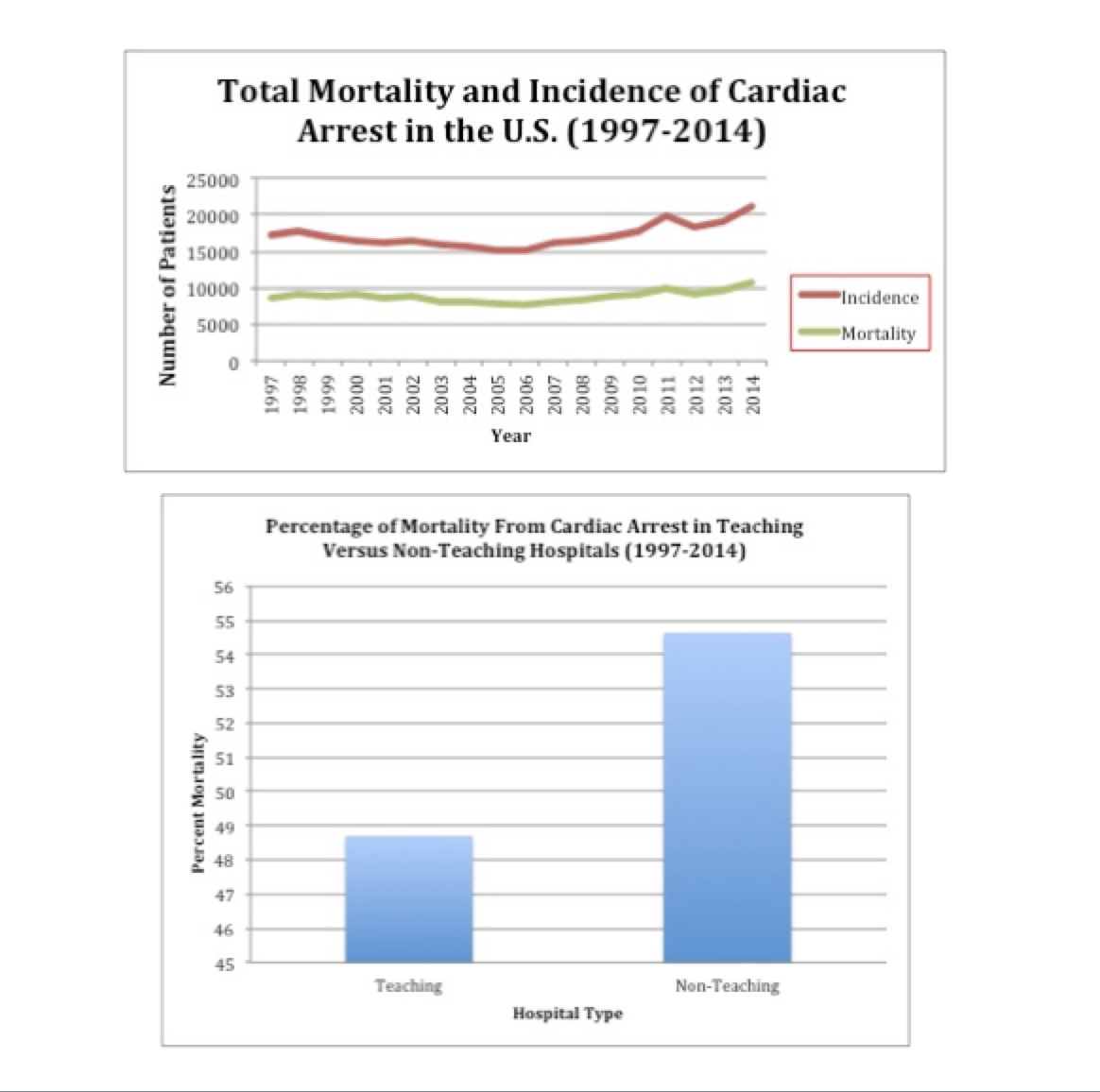
Results: Nationwide incidence of cardiac arrest in teaching and non-teaching hospitals amounted to 16,350 in 1997; this value reached a peak of 22,650 in 2014 (p <0.001). Between 1997 and 2014, the total incidence of cardiac arrests in non-teaching hospitals was 157,296, which resulted in 84,310 mortalities. During the study period, 54.6% of cardiac arrests in the Non-teaching hospitals resulted in mortality. Comparatively, the total incidence of cardiac arrests in teaching hospitals during the same period was 154,169 resulting in 75,128 mortalities. This resulted in a 48.7% mortality rate from cardiac arrest in teaching hospitals (p<0.001).
Conclusions: The total incidence of cardiac arrests from 1997 to 2014 has increased nationwide, which can be attributed to multifactorial etiologies. As demonstrated from this study when comparing percent mortality from cardiac arrest in teaching versus non-teaching hospitals, it has been determined that survivability from cardiac arrest is associated with a higher rate in teaching hospitals. Survivability from cardiac arrest relies on multiple key factors including but not limited to appropriate response time, adequate staffing, and proper administration of advanced cardiac life support. Teaching hospitals offer an increased number of trained medical staff including attending physicians, residents and nurses, which is a possible explanation to increased survivability from cardiac arrest in this setting. Further research is suggested to evaluate for medical comorbidities possibly playing a role in cardiac arrest survivability, and to improve quality of patient care in both teaching and non-teaching hospitals.