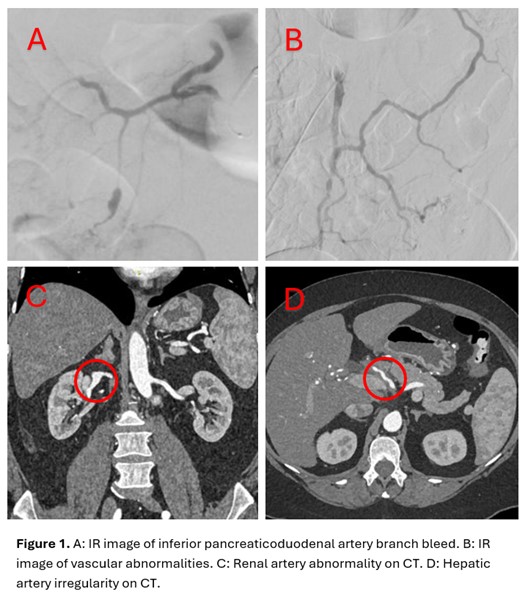
Case Presentation: A 58-year-old female presented to the emergency department with severe acute abdominal and bilateral flank pain. Medical comorbidities included hypertension and obesity.On arrival, she was hemodynamically stable and labs were notable for an elevated D-dimer. Due to concern for pulmonary embolism (PE), a heparin infusion was started. Soon afterwards, she developed acute hypotension. CTA was negative for PE and demonstrated a large retroperitoneal hematoma with active bleed.She emergently underwent embolization of an inferior pancreaticoduodenal artery branch with bleed resolution. The interventional radiology report noted diffuse mesenteric and visceral irregular vessels with ectatic, aneurysmal, and stenotic regions. This initially raised concern for vasculitis.Rheumatology work up was notable for elevated inflammatory markers all other labs (ANA, SS-A, SS-B, anti-Smith, Scl-70, Jo-1, MPO, PR3, RF, immunoglobulins, complements, cryoglobulins, SPEP) were unremarkable. A PET-CT did not show active vasculitis. CTA of the head and neck, CTA chest, and TTE did not demonstrate any significant abnormalities. A photon-counting CT revealed additional renal and hepatic artery irregularities.Leading differentials for this case of non-rheumatologic arterial abnormalities included vascular Ehlers-Danlos, segmental arterial mediolysis, Loeys-Dietz syndrome, and fibromuscular dysplasia. Genetic testing was positive for a heterozygous pathogenic variant in the TGFBR1 gene consistent with Loeys-Dietz syndrome. She met with the clinical genomics team and vascular team. She has close monitoring with abdominal CTA every 6 months and aggressive blood pressure control. Her daughter was also found to have the same mutation and is similarly monitored.
Discussion: Loeys-Dietz syndrome is a rare autosomal dominant connective tissue disorder involving mutations in the TGF-beta pathway. This typically impacts the vascular system, resulting in abnormalities like aneurysms, arterial tortuosity, and dissections. It can also cause hypertelorism, palate defects, skeletal abnormalities, easy bruising, and predisposition to allergic and inflammatory conditions.Loeys-Dietz should be suspected in patients with arterial abnormalities and/or aneurysms without another clear cause, even in the absence of other symptoms. The diagnosis is confirmed with genetic testing.These patients are at increased risk for aortic dissection and rupture of aneurysms, requiring close monitoring with head-to-pelvis imaging on a regular basis. Additionally, tight blood pressure control, typically with beta-blockers and angiotensin receptor blockers, is recommended. Genetic counseling for the patient and their family members should be offered.
Conclusions: When investigating vascular abnormalities, it’s important to keep vasculitis mimics such as Loeys-Dietz syndrome in mind as this is associated with increased risk of potentially life-threatening arterial dissections and aneurysms.