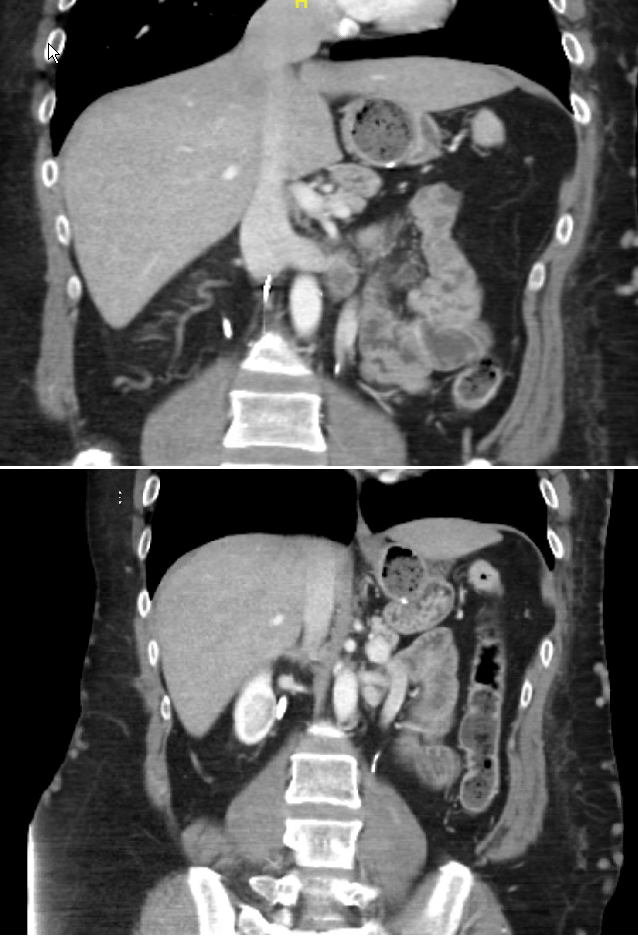
Case Presentation: A 46 year old male patient with history of Hodgkin’s lymphoma in remission, and hypercoagulable state, status post IVC-F placement in 2005 and anticoagulation. He presented with hypotension and dizziness. He has been suffering from dizziness for several months but it has been getting progressively worse, to a level that he is unable to function. On presentation his blood pressure: 85/55 mmHg, heart rate: 85 beats per minute, oxygen saturation: 100%. Orthostatic vital sign were positive with drop of blood pressure to 70/35 mmHg, and significant dizziness. The patient was admitted to the intensive care unit for suspicion of severe sepsis or septic shock. Broad spectrum antibiotics, and full infectious work up was done including negative urinalysis, chest x-ray, blood cultures, and urine culture. Laboratory work up was largely unremarkable with hemoglobin of 14 g/dl, white blood count of 5600 cells/mm³, platelets of 400,000 cells/mm³, creatinine of 1.35 mg/dl (baseline), and, normal electrolytes. As his blood pressure continued to be low but stable, lack of response to fluids, and absence of fever; antibiotics were discontinued and patient was transferred to the step down unit. Other work up included, an Echocardiogram, cortisol AM, cosynotropin stimulation test, and TSH; all within normal limits. He was started on Midodrin, fludrocortsone with no improvement of his blood pressure. He underwent a CT scan of chest, abdomen and pelvis with IV contrast that didn’t show source of an infection or bleeding, however, it showed chronic distal IVC occlusion and extensive pelvic and lumbar collateral vessels (images 1 & 2). We hypothesized that decrease preload from IVC obstruction was causing patient’s symptoms. Interventional radiology were consulted. who retrieved the IVCF, and reconstructed the IVC and bilateral common iliac veins. Post procedure; his blood pressure has improved to 95/60 mmHg. Orthostasis and dizziness resolved.
Discussion: This is an unusual case of refractory hypotension with dizziness. Possibly from decreased cardiac preload, secondary to IVC occlusion , due to thrombosis of a longstanding IVCF, given improvement after IVCF retrieval and venous reconstruction. Siew et al, reported a case of refractory obstructive shock secondary to acute thrombosis 24 hours after IVCF placement. Resolved after removal. Unlike our case this was of an immediate complication. Megri et al, reported case of refractory obstructive shock secondary to acute thrombosis of IVCF that was placed 15 years prior. Resolved after thrombectomy. Although the IVCF was placed long time ago, however, thrombosis was rather acute, which lead to shock. In our case it is likely that blockage developed slowly overtime which allowed for development of collaterals which is why patient did not develop a circulatory shock, and his symptoms were gradual. Kazuko, reported a case of acute severe leg pain, followed by hypotension, acute renal failure, and compartment syndrome in lower extremities within 20 days of IVCF placement. Due to complications and multi-organ failure care was withdrawn and patient expired. Unlike our case this one had an acute presentation with classic phlegmasia cerulea dolens.
Conclusions: In conclusoin, IVCFs have well known complications, however, this remains a rare one. Presentation could vary depending on acuity of the IVC occlusion. This reinforces the risks associated with IVCF. They should only be used as a last resort with very close follow up, and a plan for retrieval.