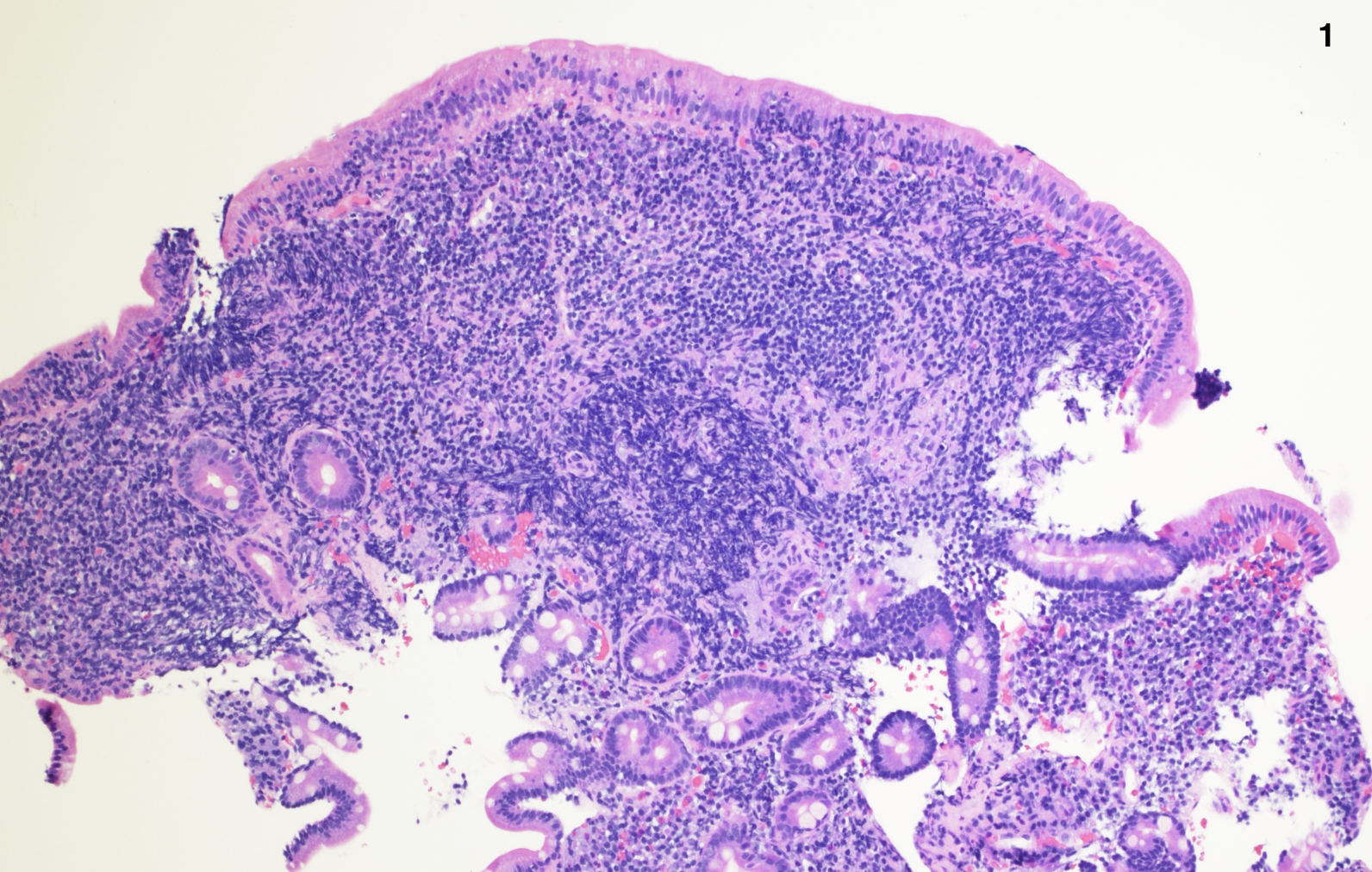
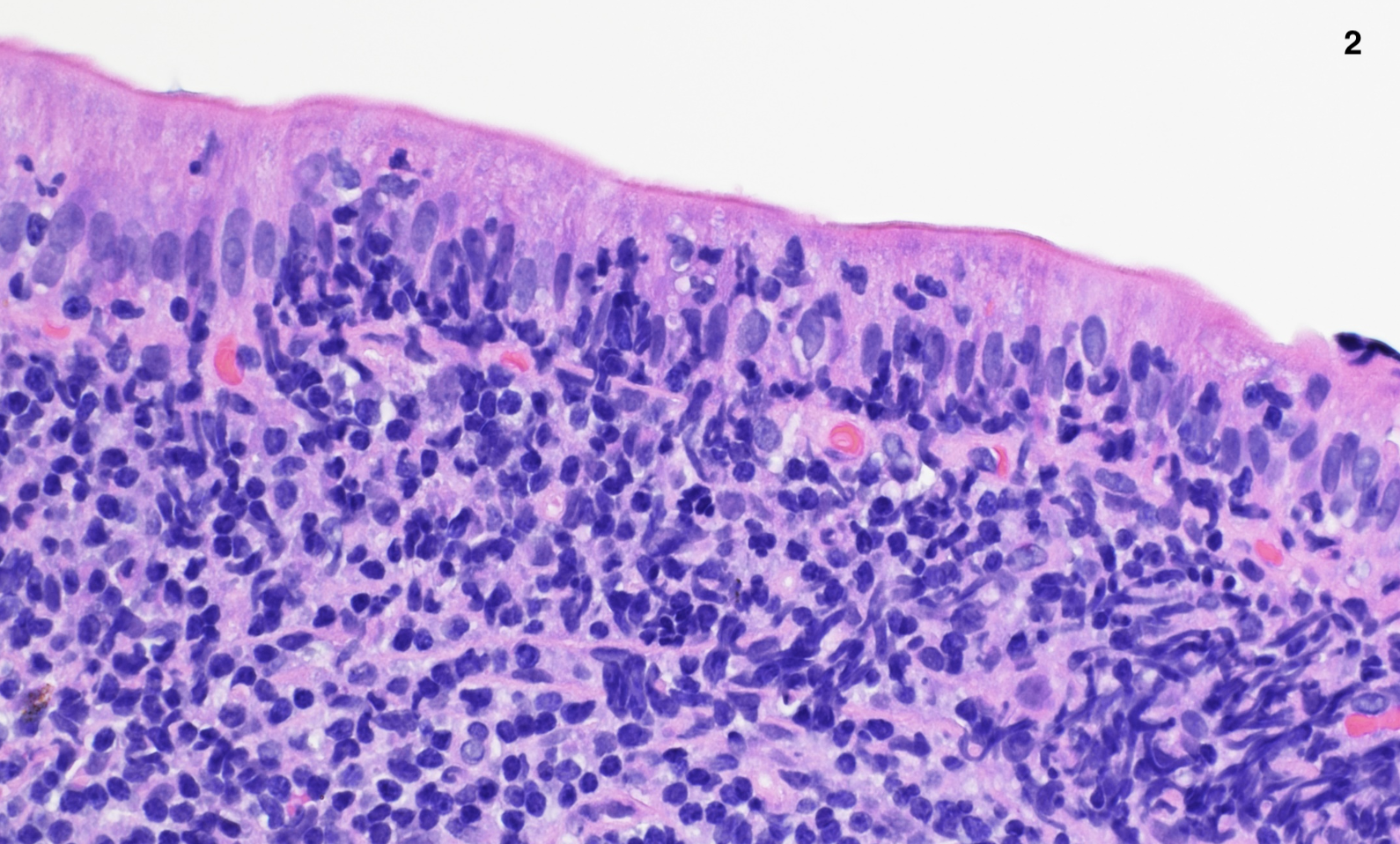
Case Presentation: A 56-year-old male with a past medical history of hypertension and diabetes presented to our gastroenterology clinic with dizziness, lightheadedness, and a feeling of being unwell since initiation of Losartan 3 months prior. Laboratory workup revealed normocytic anemia with a hemoglobin of 10.5 g/dL. He denied melena, hematochezia, abdominal pain, and changes in bowel habits. To rule out colorectal cancer and gastrointestinal (GI) bleeding, esophagogastroduodenoscopy (EGD) and colonoscopy were performed with biopsies. Visually, the esophagus, stomach, duodenum, and colon were unremarkable with no evidence of malignancy, inflammation or bleeding. Capsule endoscopy was also unremarkable. A subsequent iron panel revealed iron deficiency anemia (iron 38 mcg/dL, ferritin 20 ng/mL), and he was started on oral iron. Biopsies eventually showed villous blunting with inflammation in the first portion of the duodenum as well as foci of increased intraepithelial lymphocytes. Subsequent serological workup with tissue transglutaminase IgA ruled out celiac disease. Considering the negative workup and high suspicion for angiotensin type 1 receptor blockers (ARBs) induced enteropathy, the patient’s losartan was discontinued and, after six weeks, his anemia resolved.
Discussion: In recent years, a phenomenon involving ARBs leading to sprue-like enteropathy in the absence of celiac disease, has been increasingly observed. In 2019, a meta-analysis revealed a class-wide enteropathic effect involving ARBs. Patients typically report abdominal pain, chronic diarrhea, and weight loss. Endoscopically, mucosal inflammation is visualized, with duodenal villous atrophy present histologically. Particularly among patients using Losartan, anemia is observed alongside GI symptoms. Our patient presented uniquely with anemia in the absence of any GI symptoms. Additionally, most patients have visible duodenal mucosal inflammation on EGD, whereas our patient only demonstrated villous blunting, seen histologically. When suspecting ARB-induced enteropathy, celiac disease must be ruled out due to overlapping histological patterns. In our case, both celiac disease and GI bleeding were ruled out. Eventually, six weeks following discontinuation of Losartan, our patient had symptom resolution, with normalization of hemoglobin (13.8 g/dL) and ferritin (24 ng/mL). Iron levels improved to 38 mcg/dL.
Conclusions: Since the first case report of Losartan-induced sprue-like enteropathy in 2015, the number of cases of ARB-induced enteropathy has been increasing. While enteropathy should be highly suspected in patients with chronic diarrhea and weight loss while on an ARB, it is important to note that patients can present atypically and be devoid of any GI symptoms. Additionally, new onset of anemia following initiation of an ARB should warrant workup with EGD and biopsy to assess for sprue-like enteropathy followed by serology to rule out celiac disease.