Background: Heart Failure (HF) is among the top 10 causes of hospitalization and almost a fifth are readmitted within 30 days. Clinical assessment of lung congestion is subjective and patients may be discharged prior to good resolution. Lung ultrasound (LUS) is helpful in evaluating lung congestion. The presence of B-lines on LUS can reliably indicate pulmonary edema. Prior studies have shown that B-lines resolve with inpatient therapy of HF. There is limited data on whether using LUS to guide inpatient HF therapy impacts readmissions. We aim to determine whether a simplified LUS-guided strategy to manage HF reduces the risk of HF-related readmissions.
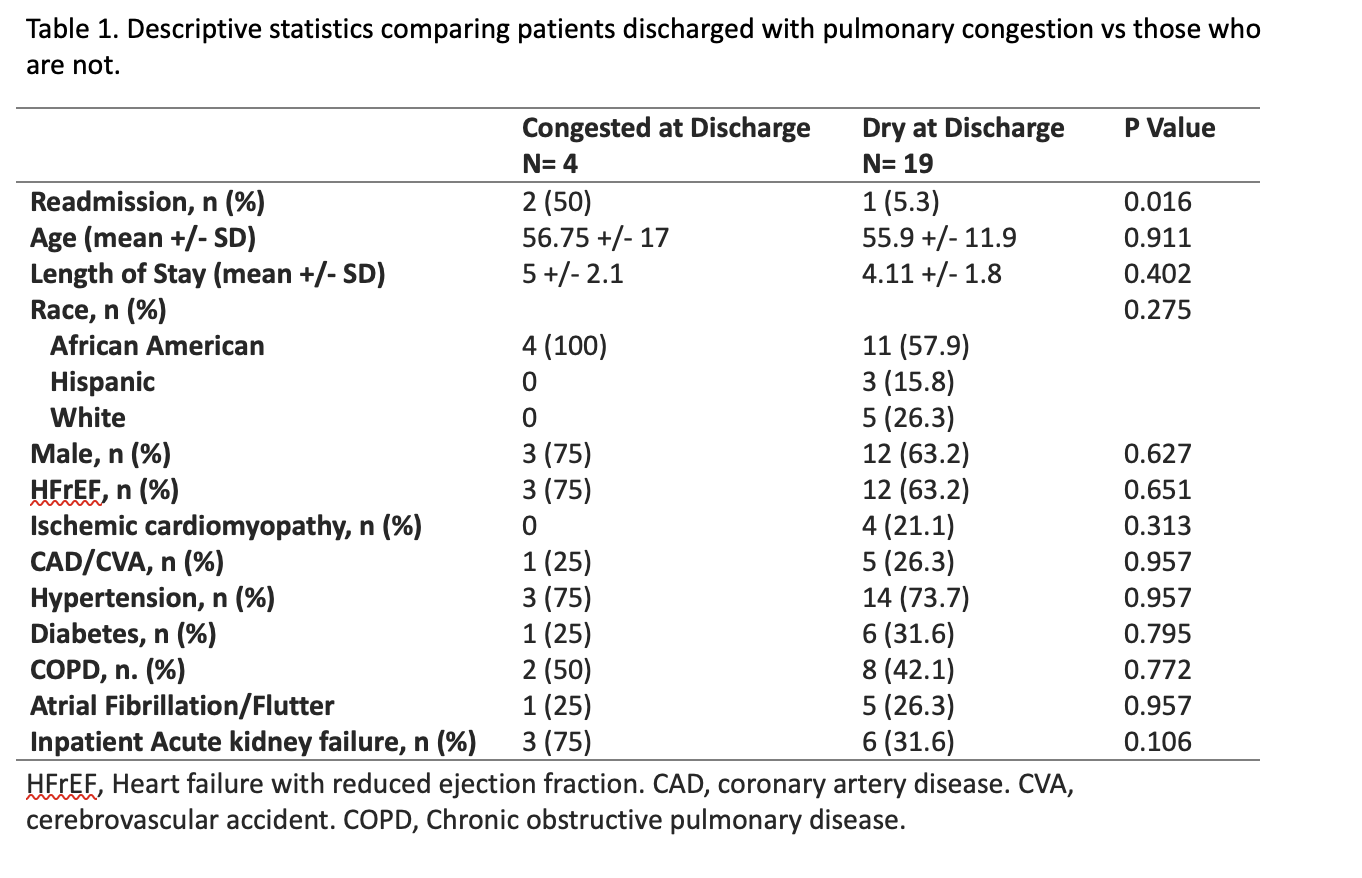
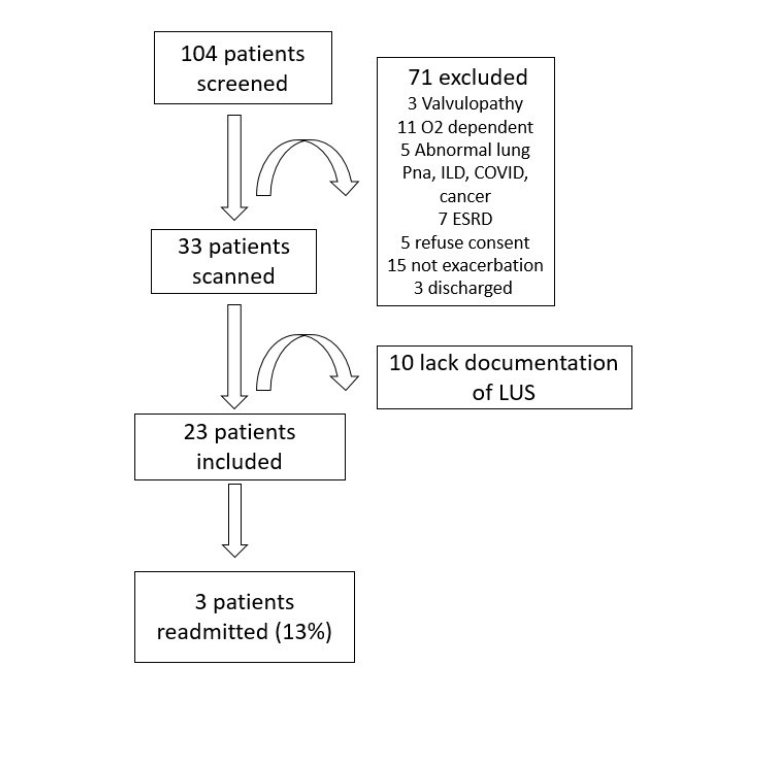
Methods: Patients with a HF-related diagnosis codes were screened for eligibility. Informed consent was obtained from eligible patients who underwent LUS with a General Electric Venue machine. An established 8-zone scanning protocol was used. A B-line was defined as a discrete vertical hyperechoic artifact starting at the pleural line and extending to the end of the screen without fading. Three or more B-lines was defined as a positive zone. A single large B-line was considered positive if occupying more than 30% of the field. Congestion was defined as present if 2 zones in each hemithorax were positive. Study investigators with point of care ultrasound (POCUS) training proctored 10 scans performed by each resident to ensure inter-observer reliability. LUS examinations were done until no more congestion was observed. Primary teams were contacted via hospital encrypted messaging system and findings were documented in the Electronic Medical Record. We advised continuing intravenous therapy if patient was congested, and switching to oral if not. Teams could opt to use the recommendations. Chart review was done to obtain demographics, comorbidities, congestion at discharge, medical team decisions and 30-day readmissions. Data was analyzed using IBM SPSS Statistics 26. Categorical variables were compared using chi squared and numerical values were analyzed using means +/- standard deviation and the statistical significance was obtained using ANOVA.
Results: 104 patients were screened, 71 were excluded and 33 met inclusion criteria. Only 23 had documentation of LUS findings so were included in the final analysis. Out of the 23 patients included, 4 (17.4%) were congested at discharge, 9 (39.1%) developed inpatient acute kidney injury (AKI) and 3 (13%) were readmitted within 30-days. 65.2% had HF with reduced ejection fraction. 4 out of 23 patients were discharged despite congestion on LUS. Of these discharged patients, 50% returned within 30-days with HF symptoms. Of the 19 that were discharged without congestion, only one was readmitted due to AKI. The readmission rate in the non-congested group was 5%. 9 out of 23 patients developed AKI. 4 out of 9 cases of AKI could have been prevented if the team switched to oral therapy as advised. 3 out of 4 patients in the congested group developed inpatient AKI. One was due to ACE-inhibitor use and the other was contrast-induced. Only one case was attributed to over-diuresis. Mean length of stay (LOS) was 5 +/- 2 days vs 4.1 +/- 1.8 days, in congested vs not congested patients. The initial scans were done by residents with supervision, the later scans were done unaided.
Conclusions: The readmission rate in our patient population was 13% compared with a baseline of 25%. Using LUS with inpatient HF therapy reduces pulmonary congestion at discharge which may decrease 30-day HF readmissions and readmissions due to AKI, without significantly increasing LOS.