Background: A problem list serves as a central place for hospital-based clinicians to obtain a comprehensive and concise view of the patient’s active medical conditions. Use of the hospital problem list has many potential benefits: it provides a mental model of patient’s health status; streamlines the documentation process; makes chart review more efficient; facilitates communication between inpatient and outpatient clinicians; and has the potential to reduce medical errors due to omission of key clinical information. Further, it streamlines coding and billing processes and can facilitate research studies. Despite these advantages, use of this tool remains suboptimal. The purpose of this study was to explore patterns of use of the electronic health record (EHR) based problem list tool to gain insights about how, when, why, and by whom it is used during the hospital encounter.
Methods: The study was conducted at a large academic medical center that uses Epic’s EHR system. The software has a problem-based charting tool that facilitates structured entry and management of active problems identified during the hospital encounter. We used REDCap to survey a random sample of attendings, advanced practice providers (APPs) and internal medicine residents. The survey assessed clinicians’ patterns of use of this tool, and factors that positively and negatively impacted its acceptance. We sought feedback regarding what would make providers more likely to incorporate EHR-based problem lists in their workflow. Descriptive statistics were used to report survey responses and qualitative analyses were done to further understand our findings.
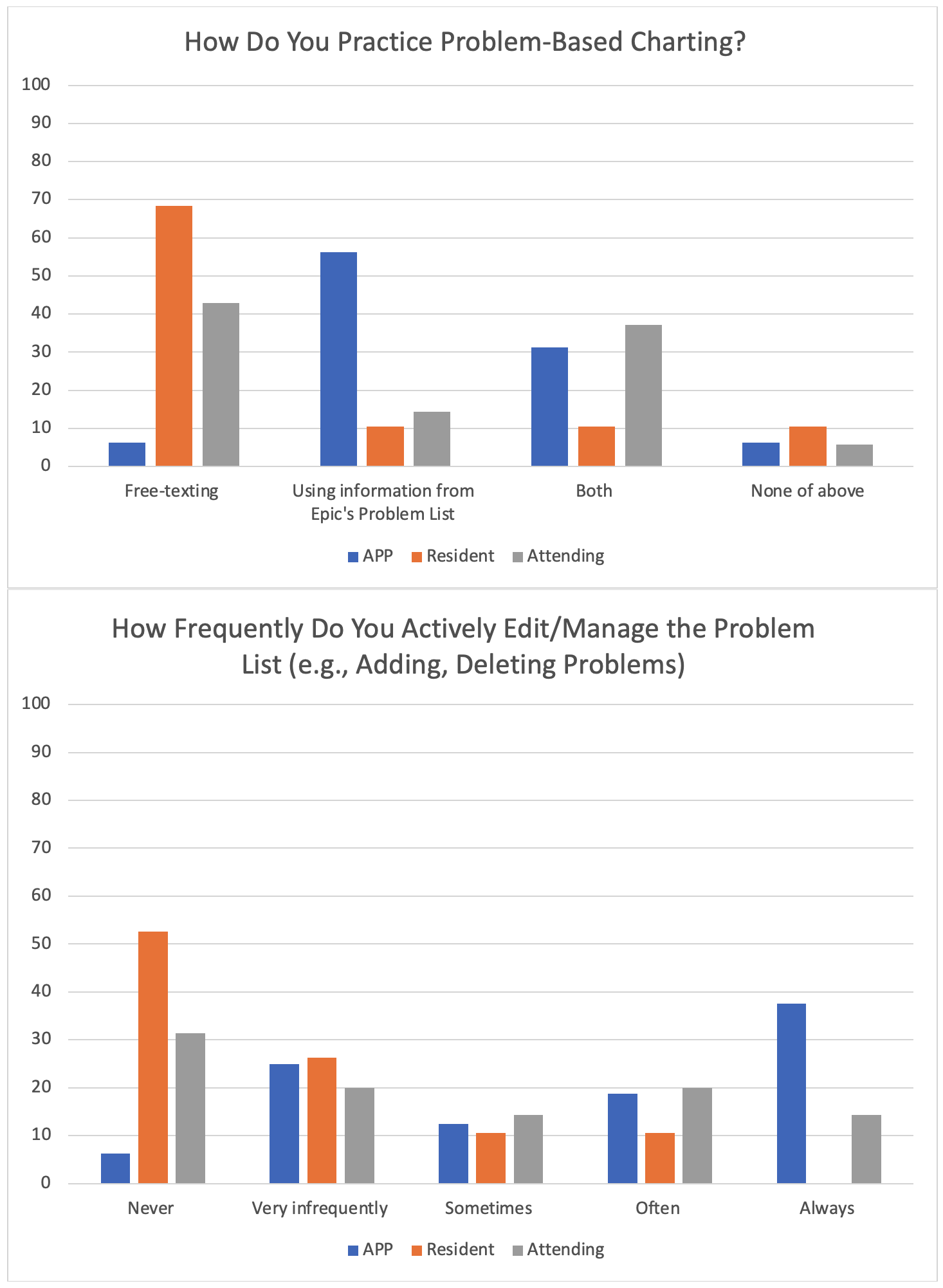
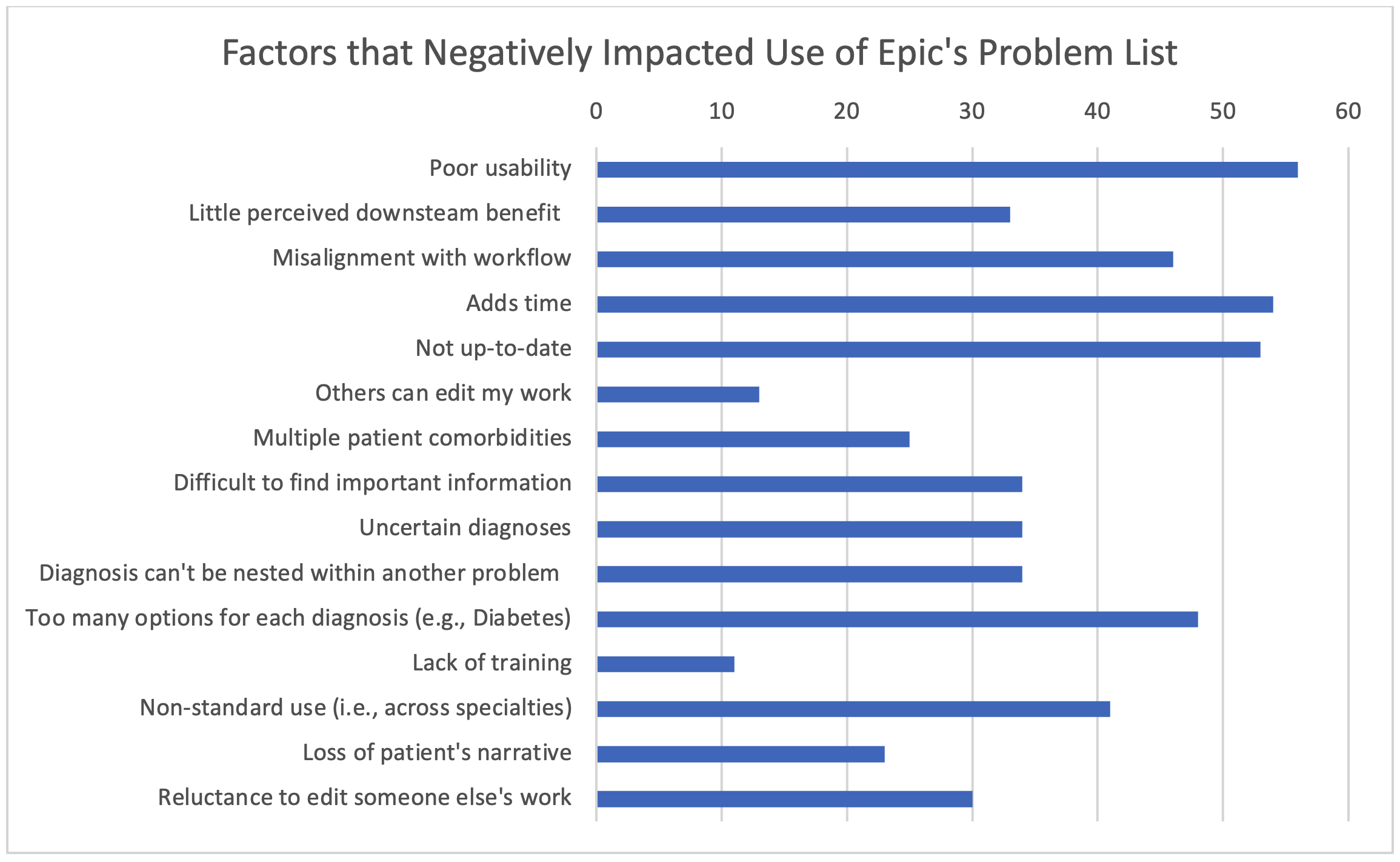
Results: Of the 185 clinicians who were sent the survey, 102 (55.1%) submitted their responses (mean age 38.5 years, 50.0% female, 22.9% APPs, 27.1% residents, 50.0% attendings). Fifty-five (53.9%) respondents stated that they never or rarely edited the EHR-based problem list. Of the 47 users who actively edited/managed the problem list, 63.8% reported doing so at the time of admission. EHR-based problem list tool was most consistently used by APPs, while residents preferred free-texting instead (Figure 1). Most often cited benefits of using problem lists were identifying/managing chronic conditions (67.5% users) and ability to auto-populate progress note templates (65.7% users). Most commonly reported barriers (Figure-2) were poor usability (54.9%), time constraints (52.9%), and old problem lists not being up to date (52.0%). Key feedback from residents about what would improve acceptability included: clear usage guidelines as part of orientation; similar guidelines for outpatient providers to keep lists up to date; and improvements in EHR user interface that would require ‘less clicks’.
Conclusions: In this study at a large academic medical center, we found significant variability in patterns of use of problem lists among different types of hospital-based clinicians. Medicine residents were least likely to actively manage EHR-based problem lists, while APPs used the tool most effectively, especially at the time of admission. Poor usability, time constraints, and inconsistent adoption across settings were key barriers. Better EHR tools (e.g., with drag and drop functionality to manage lists), appropriate education and training, and standardization of usage guidelines across departments and institutions, would likely increase acceptance. Consistent use of EHR-based problem lists, in turn, would make clinical documentation more efficient and reduce medical errors.