Case Presentation:
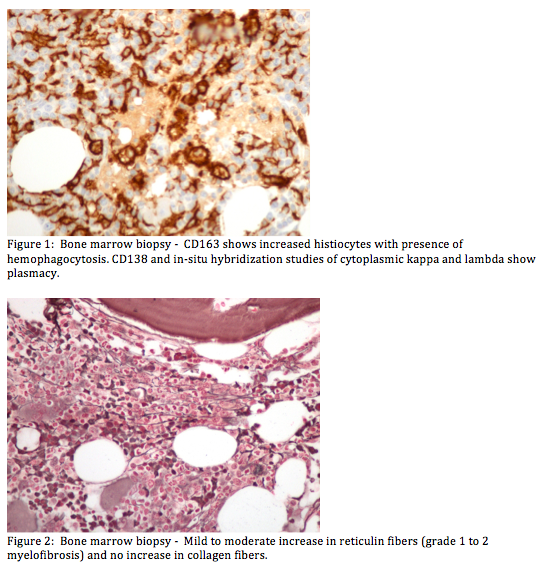
A 55 year-old African American woman with history of SLE (on cellcept and plaquenil) and history of cervical cancer (s/p TAH-BSO in 2003) with celiac lymphadenopathy and recently diagnosed hepatic metastases, presented with acutely worsening diarrhea and malaise for 3 weeks prior to admission. She was noted to have diffuse abdominal tenderness on exam and labs revealing pancytopenia with autoimmune hemolytic anemia and coagulopathy. Peripheral smear showed moderate anisocytosis and macrocytosis, with slight poikilocytosis, tear drops, and schistocytes. Ferritin was elevated (752mg/dl). She had persistent low-grade fevers with no clear etiology and supportive care was provided with empiric antibiotics and pRBC, plaletet, and cryopreciptate transfusions. RVP, CMV, Parvovirus, HIV, hepatitis panel, blood and stool cultures were negative. Patient also had low C3, C4, and elevated DsDNA, concerning for lupus flare. She was started on prednisone 60mg BID. A bone marrow biopsy revealed hemophagocytosis and autoimmune myelofibrosis, consistent with systemic lupus, and no evidence of acute leukemia or lymphoma. Given these results and the patient’s clinical presentation notably fever, cytopenia, hypofibrinogenemia, and elevated ferritin, there was concern for lupus induced hemophagocytic lymphohistiocytosis (HLH). She was started on pulse dose solumedrol for three days. The patient subsequently developed altered mental status, and a CT head showed intracerebral hemorrhage in the left occipital, left fronto-cortical, right temporal, and left subdural regions. She was transferred to intensive care unit where she expired 3 days later.
Discussion:
We present a case of lupus induced HLH without any evidence of lymphoma or leukemia. Our patient met five of the eight diagnostic criteria, including peripheral cytopenia, hypofibrinogenemia, hemophagocytosis in bone marrow, ferritin>500, and fever. Standard treatment of HLH involves dexamethasone, etoposide, and intrathecal methotrexate for 8 weeks. For patients with an underlying cause for HLH, such as infection, malignancy, or rheumatological disease, treatment is targeted at the underlying problem. Given the evidence for hemophagocytosis in the setting of positive markers for lupus flare, our patient was started on pulse doses of steroids. However the ongoing consumptive coagulopathy and possible lupus flare with notable signs of cerebritis may have contributed to her unfortunate outcome.
Conclusions:
Usually the result of an infection, adult HLH is rarely associated with SLE. Here we present a case of lupus induced HLH with possibly active lupus cerebritis, who decompensated after having a spontaneous ICH. Survival with treatment for HLH has been estimated at 55%. SLE associated HLH typically portends a poor prognosis.