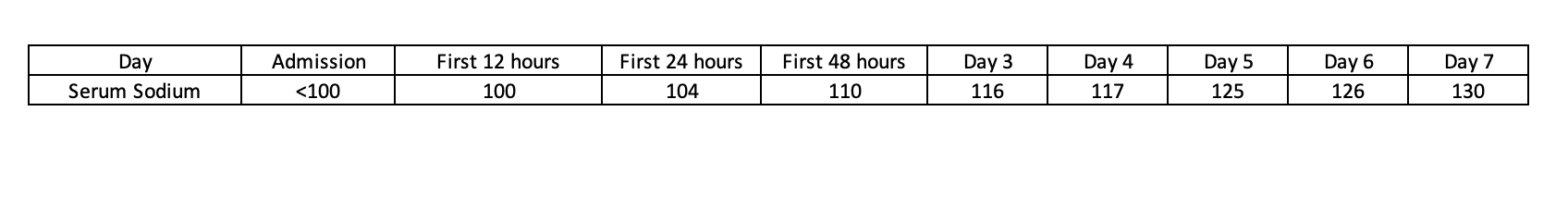
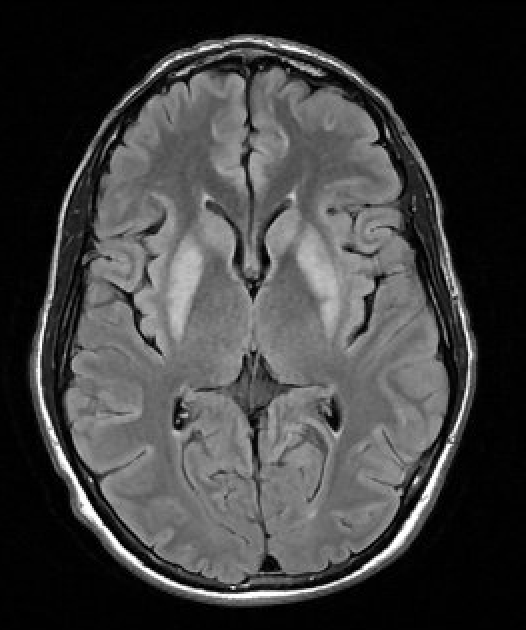
Case Presentation: A 34-year-old man with hypertension on chlorthalidone and recent COVID-19 infection treated with Paxlovid presented to the ED with three days of shortness of breath, dizziness, and diarrhea. On exam, he was alert, neurologically non-focal, and underweight by BMI. Initial lab work was significant for severe hyponatremia (< 100 mmol/L) and hypokalemia (2.3 mmol/L). Serum osmolality was very low (199 mOsm/kg) and urine osmolality and random urine sodium were inappropriate (486 mOsm/kg and 50 mmol/L, respectively). Cortisol and TSH levels were normal. He was admitted to the ICU for hypertonic saline infusion and careful correction of severe, subacute SIADH in the setting of chronic thiazide diuretic use compounded by COVID-19 infection. Over the course of 9 days, the serum sodium was slowly corrected with a delicate balance of desmopressin and sodium chloride tablets. He remained clinically asymptomatic and was discharged home with a sodium of 132 mmol/L. Three days later, the patient returned with worsening fatigue, slow speech, and involuntary clenching of the hands and jaw. Serum sodium was 137 mmol/L. A contrast brain MRI revealed symmetrically increased T2 signal affecting the bilateral basal ganglia with mild diffusion weighted hyperintensity without post-contrast enhancement consistent with osmotic demyelination syndrome (ODS). He declined a trial of plasmapheresis. Baclofen and Klonopin were given for dystonia and he was discharged to an acute rehabilitation facility. Two months after discharge, a follow-up brain MRI remains unchanged but the patient is clinically improved and reported no residual gross neurologic or physical deficits.
Discussion: The prevalence of osmotic demyelination syndrome is estimated to be 0.25-0.5%. Risk factors include a serum sodium ≤105-110 mmol/L, duration of hyponatremia longer than 2-3 days, malnutrition, concurrent hypokalemia, female gender, alcohol use disorder, liver cirrhosis, and overly rapid correction. The onset of clinical manifestations is often delayed and range from dysarthria, dysphagia, and movement disorders to seizures, obtundation and coma. Pontine and/or extra-pontine demyelination on MRI with a corroborative clinical history and exam are diagnostic. Given the variable reported long-term neurologic outcomes of patients with ODS, employing protective strategies in hyponatremia management are paramount. Sodium rise should be limited to < 8 mmol/L in a 24-hour period and < 18 in any 48-hour period. Concurrent use of desmopressin can help mitigate over-correction. Management strategies for ODS include acute re-lowering of sodium within 8-10 hours of symptom onset and supportive care. Case reports suggest clinical benefit from plasmapheresis, which is thought to remove pro-inflammatory myelinotoxins. Our patient had at least 4 identified risk factors for ODS and despite careful and appropriate correction of his hyponatremia, osmotic demyelination still developed.
Conclusions: We present a case of severe, subacute SIADH in a young patient whose management was complicated by osmotic demyelination syndrome. Theoretical medicine forms the basis for guideline directed practice, but real-world outcomes can deviate from expectations and the text. We are reminded that each case of sodium correction should be delicately approached and that practice guidelines offer risk-reductive strategies but do not eliminate the risk of ODS.