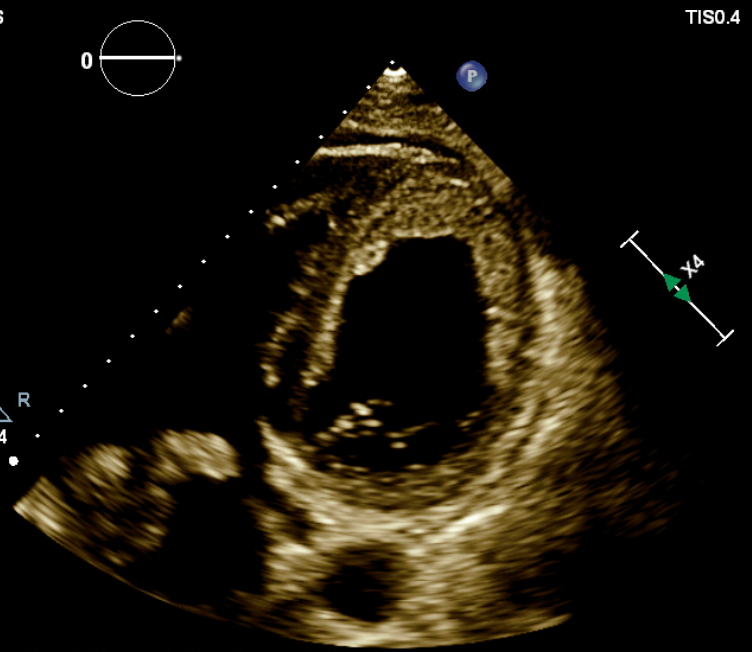
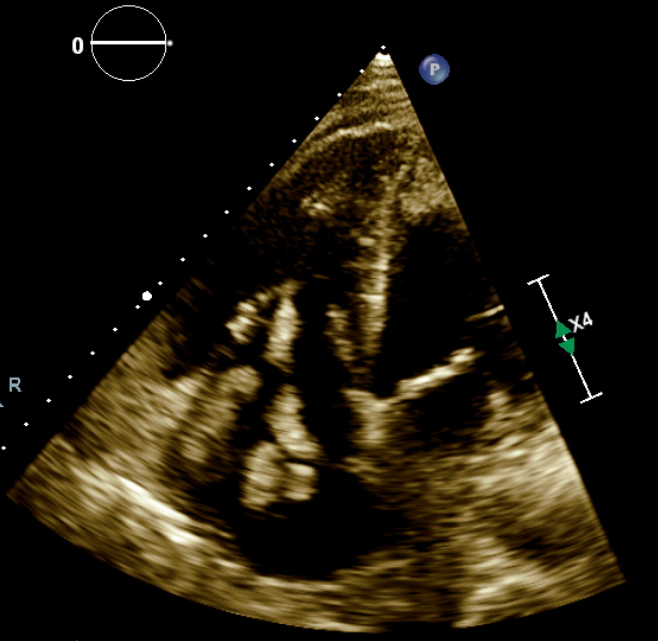
Case Presentation: The patient is a 58-year-old African-American male with no known past medical history. He presented to the emergency room complaining of shortness of breath. He had been at home taking care of his parents, who were both COVID-19 positive, for the past four weeks. He reported that he has been feeling unwell since then. The initial vital signs revealed; blood pressure 108/64 mmHg, respiratory rate 32/min, heart rate 122 beats/min, fever 98.1 F, oxygen saturation 60% on room air. Lung examination revealed bilaterally diminished breath sounds. Significant swelling and tenderness in the right lower extremity were found. The rest of the physical examination was unremarkable. Complete blood count showed lymphopenia. The D-dimer level was > 20 ug/mL. A chest X-ray showed extensive patchy bilateral alveolar findings compatible with viral pneumonia. The BNP level was 34824 pg/mL. Due to acute hypoxic respiratory failure, the patient was intubated and admitted to the critical care unit. Initial SARS–CoV-2 PCR testing was negative in nasopharyngeal swab; however, given the strong suspicion of COVID-19 pneumonia, a repeat test was sent, and the patient remained isolated. He was found to have extensive right leg deep vein thrombosis in the right common femoral vein, right popliteal vein, right posterior tibial vein, right peroneal vein, right gastrocnemius, and right small saphenous vein. The CT Angiography of the chest showed bilateral pneumonia with large right pleural effusion, and biventricular thrombi but negative for actual pulmonary embolism. The transthoracic echocardiography showed an ejection fraction of 10% to 15% with biventricular failure and severe global hypokinesis. There was an extensive mural thrombus seen along all walls of the left ventricle (Figure 1). Also, there was a mobile worm-like thrombus in the right atrium with an extension across the tricuspid valve into the right ventricle (Figure 2). The hypercoagulability panel was within normal limits. Anticoagulative treatment was initiated. Unfortunately, he had a cardiac arrest due to persistent ventricular fibrillation and was unable to be resuscitated. He expired within 24 hours of admission.
Discussion: Recent clinical data showed that the coronavirus disease 2019 (COVID-19) is associated with a hypercoagulable state and predisposes to thrombotic complications. Notably, distinct coagulation activation is correlated with cardiac injury and increases mortality. COVID-19 is an emerging threat due to the risk of microvascular, venous, and arterial thrombosis, thereby exacerbating organ injury and mortality. Although the exact mechanism of extensive thromboembolism and myocardial injury caused by SARS-CoV-2 is not illuminated, it is clear that COVID-19 related hypercoagulation increasing the fatality of the disease.
Conclusions: Based on the current data, we urge awareness of severe and potentially fatal extensive thrombosis and cardiac failure as the initial clinical presentation of possible SARS CoV 2.