Background: Medication errors are common, with more than half of patients estimated to have greater than or equal to one unintended medication discrepancy at hospital admission. Medication reconciliation can identify errors. Although there has been significant investigation into the most effective logistical strategies for performing medicine reconciliation within the healthcare system, there is little investigation into teaching these skills to medical students and the direct impact on medication management in the hospital.
Purpose: Develop and implement a skills-based curriculum for students to: 1) apply skills in patient interviews to obtain a medication history (best possible medication history or BPMH), 2) identify medication errors, 3) assess for facilitators and barriers to medication safety and 4) provide recommendations to the primary team.
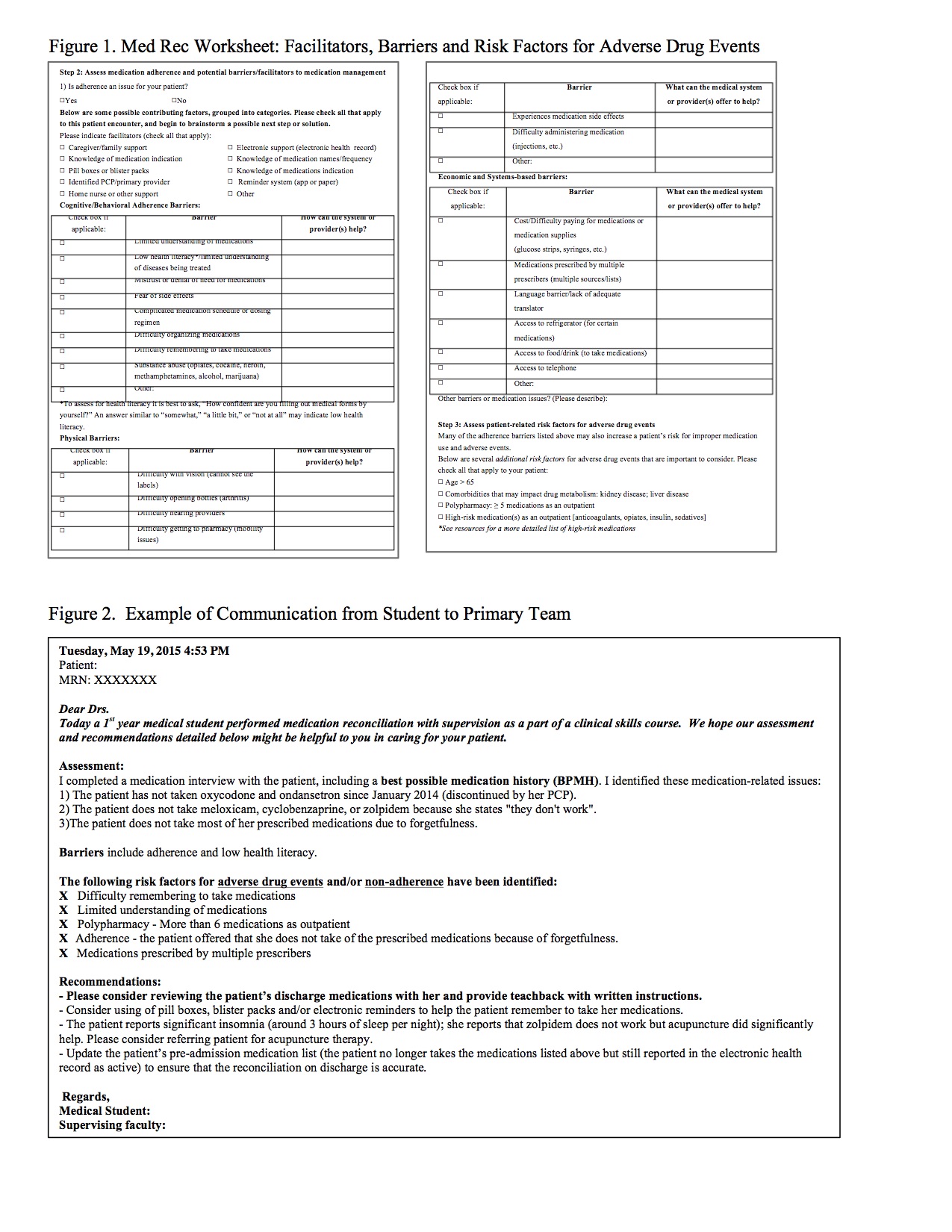
Description: The curriculum was piloted with six 1st year medical students in 2014 and 15 students in 2015 at 3 hospitals within a university system (tertiary care center, county hospital and VA hospital). Over the course of 10 half-day sessions students met with a faculty facilitator and identified patients for medication reconciliation. Using a “med rec” worksheet each student performed at least one patient interview per session completing the BPMH including all medication discrepancies and identified facilitators and barriers to medication management (e.g. adherence, cost, polypharmacy) (Figure 1). The students contacted the primary hospital providers using a templated communication form, including recommendations regarding patient-reported barriers (Figure 2). On average students identified 2.3 medication errors per patient encounter and at least one barrier. Compared to pre-survey findings, there was a measurable improvement in student’s knowledge and skills. Using a 5-point Likert scale, all of the students in follow up agreed or strongly agreed that they applied these skills during their clinical rotations. Students independently identified several areas involving the electronic health record and communication between providers as potential gaps in systems-based practice. Hospitalist faculty and residents highly rated the student communications to the primary team and identified a plan to implement at least one of the recommendations.
Conclusions: This skills-based curriculum embedded early medical students into the workplace with value added to a critical patient safety activity. The curriculum provided a systematic and comprehensive approach to medication reconciliation and medication safety. In learning skills such as medication reconciliation, early medical students can directly impact patients and contribute to systems-based care.