Background: Unlike other chronic conditions such as diabetes mellitus and heart disease, substance use disorder (SUD) has only recently been recognized by the medical community recently as a medical condition, and stigmatizing beliefs have lingered. Formal teaching about SUD has been shown to foster a more positive attitude towards these patients among medical trainees. Attitudes pertaining to the care of patients with SUD are informally and implicitly taught during medical training through language, behaviors, and actions, and they shape medical trainees’ attitudes and behaviors. Our objective is to explore how medical students perceive the way the professionals with whom they worked clinically cared for patients with SUD.
Methods: For this qualitative study, 60 medical students at our institution who had completed their core clerkships at any affiliated site were identified using a random number generator; 13 agreed to be interviewed. Via semi-structured interviews, we interrogated how respondents perceived the attitudes towards patients with SUD among clinical teams with whom the respondents worked on their inpatient and outpatient rotations. Respondents were interviewed for 20 to 30 minutes via Zoom videoconferencing, then transcripts were reviewed and coded by three members of our research team using thematic analysis. There was overall concordance between reviewers in these double-coded interviews, with discrepancies resolved via discussion. Thematic saturation was reached after 13 interviews.
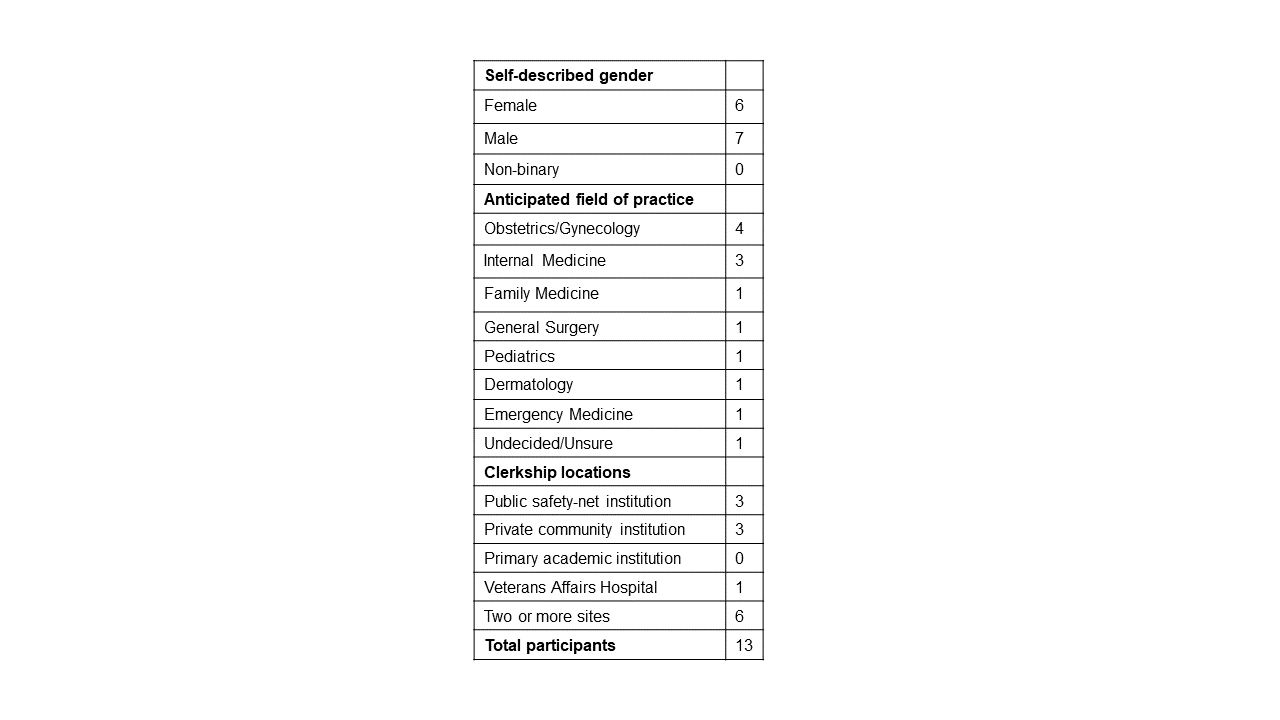
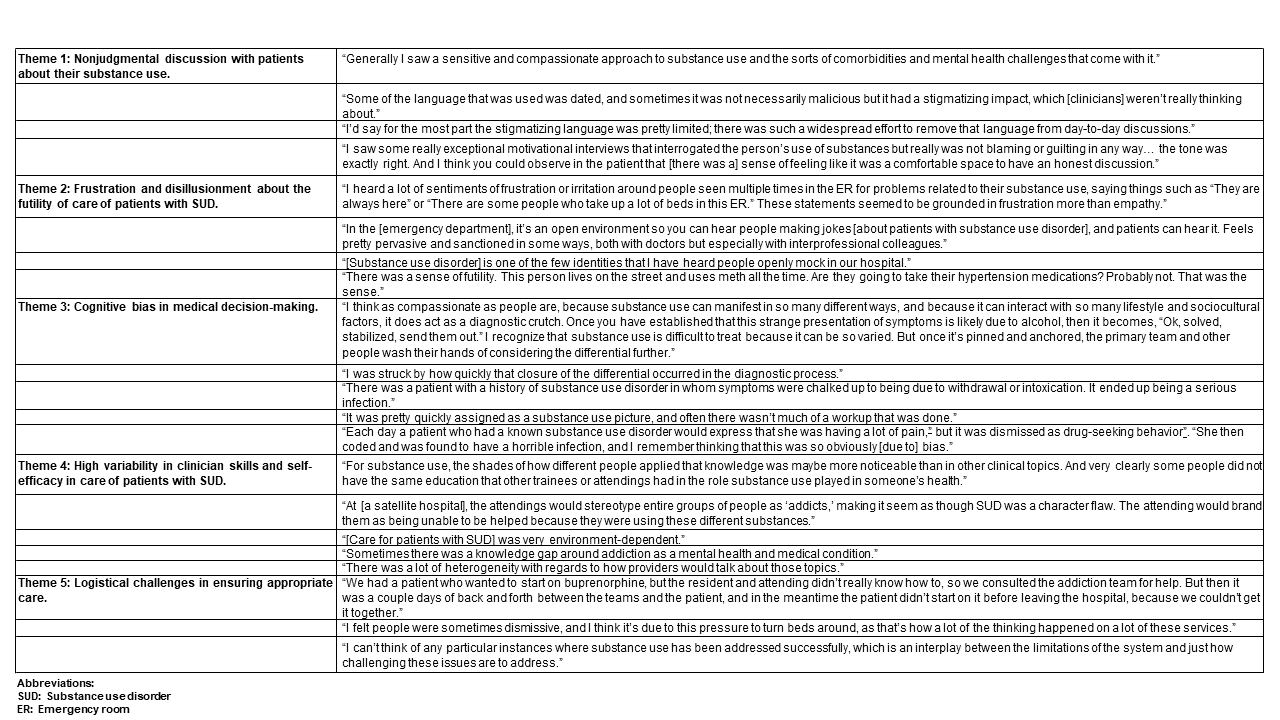
Results: Participants’ demographics, the clinical sites at which participants rotated, and participants’ future fields of study are listed in table 1. Dominant themes were as follows: 1) Students perceived nonjudgmental discussion between providers and patients about substance use; 2) Students perceived that some clinicians were frustrated and disillusioned about the perceived futility of care of patients with SUD; 3) Students perceived cognitive bias in medical decision-making and subsequent negative effects on patients’ medical care; 4) Students perceived high variability in clinician skills and self-efficacy in the care of patients with SUD; and 5) Students perceived that the care team faced logistical challenges in ensuring optimal care for patients with SUD (Table 2).
Conclusions: This study of medical student perceptions of the care of patients with SUD indicates that although many physicians treat patients respectfully and appropriately, in line with formal curricula on this topic, challenges remain with regards to lingering stigmatizing beliefs. In addition, obstacles related to medical decision-making and to the provision of adequate resources in the care of these patients must be addressed. Further research is needed to assess whether the themes identified in our study are generalizable to other institutions and geographic locations.