Background: Consultation among providers is a foundation of modern health care and a very frequent means of interdisciplinary communication. Classifying consultation requests can facilitate clear communication between providers and across medical specialties, improve workflow, provider satisfaction and ultimately patient care. We previously proposed an organizing framework of 7 specific consultation types: ideal, obligatory, procedural, S.O.S., confirmatory, inappropriate, and curbside.1 Here, we sought to validate this framework by classifying real-world consultation requests and using focus groups across 5 medicine subspecialties.
Methods: In this mixed methods study, 100 random consult requests were extracted from the electronic medical record from 5 medicine subspecialties (Hematology, Infectious Disease, Nephrology, Gastroenterology and Pulmonary Medicine) and anonymized. Three hospitalists and 3 specialists from each of the respective specialties were recruited. Participants attended focus groups that described the consulting framework and prompted a semi-structured discussion that was recorded, transcribed and subsequently coded for thematic saturation. Each specialist categorized the consult requests from their respective specialty using the proposed framework, and each hospitalist categorized all 500 consult requests. The primary outcome was concordance in classification of consult requests, defined as the sum of partial concordance and perfect concordance. Partial concordance was reached when 4-5/6 participants classified a consult in the same category. Perfect concordance was reached when all 6/6 individuals classified a consult in the same category. We hypothesized that there would be at least 70% concordance overall. We used chi square tests to compare rates of concordance across specialties and between specialists and hospitalists.
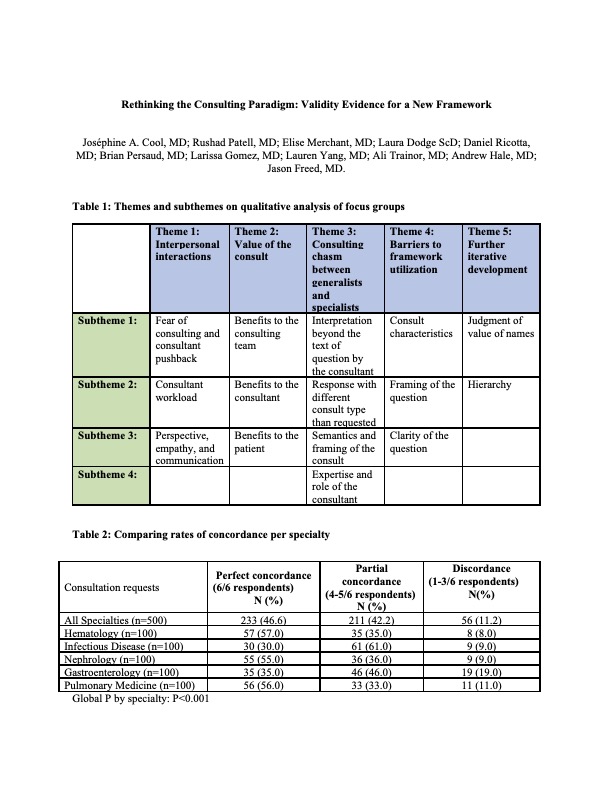
Results: In the qualitative analysis of the focus groups, the major themes identified included: interpersonal interactions, value of the consult, consulting chasm between specialists and generalists, barriers to framework utilization and further iterative development. (Table 1) Providers from all specialties agreed that the current consulting status quo lacks generalizability and can lead to miscommunication and frustration. The consulting framework was found to be useful by most providers in terms of augmenting communication, efficiency and education.The overall rate of concordance was 88.8% (95% CI: 85.7-91.4), and perfect concordance was 46.6% (95% CI: 42.2-51.1). Within-specialty concordance rates were significantly different when compared across specialties (P< 0.001). Hematology (57%) and Nephrology (55%) had the highest perfect concordance, and Gastroenterology (35%) and Infectious Diseases (30%) had the lowest. (Table 2) Concordance differed significantly between hospitalists and specialists overall (P=0.01), with a higher proportion of hospitalists having perfect (3/3) concordance compared to specialists (67.2% vs. 57.8%, P=0.002).
Conclusions: The proposed consulting framework was successfully validated using a mixed methods study, with 89% concordance across specialties. The framework was also found to have benefits in consultative medicine that go beyond patient care and include improved communication and education. Integrating a validated framework to classify consultation requests can be used to improve consultative efficiency.