Background: Third and fourth year medical students’ experience on general internal medicine ward teams is an integral part of medical student education. At many institutions this experience includes participation in unit based Care Coordination Rounds (CCRs), including our own. These daily multidisciplinary discharge planning meetings are ubiquitous, however students are often uncomfortable presenting at these meetings as they do not receive structured training in participating in CCRs. Students reported feeling unprepared to participate, and members of patient care teams reported suboptimal student performance when participating in daily care rounds. We developed a 30 minute interactive curriculum to improve medical students’ understanding of, and performance in, CCRs. The components of the curriculum were derived from a systematic needs assessment covering students, course directors, charge nurses and social workers on general internal medicine floors.
Methods: Students were divided into intervention (N=59) and control groups (N=26), with the intervention group receiving the curriculum at the beginning of the ward month and the control group receiving the curriculum at the end. The curriculum discussed the purpose of CCRs, the specific participants present and their roles, and the expected content of presentations. Sample cases were broken down and discussed, with students participating in role play as CCR participants. Anonymous pre- and post-curriculum surveys were given to assess students comfort level with, and knowledge of, the curriculum content. In addition to student focused evaluations, charge nurses completed a standardized checklist assessing medical students’ performance at CCRs. The checklist covered presentation of the patients’ reason for admission, barriers to discharge, expected discharge date, and students’ ability to answer questions about the multidisciplinary aspects of the case.
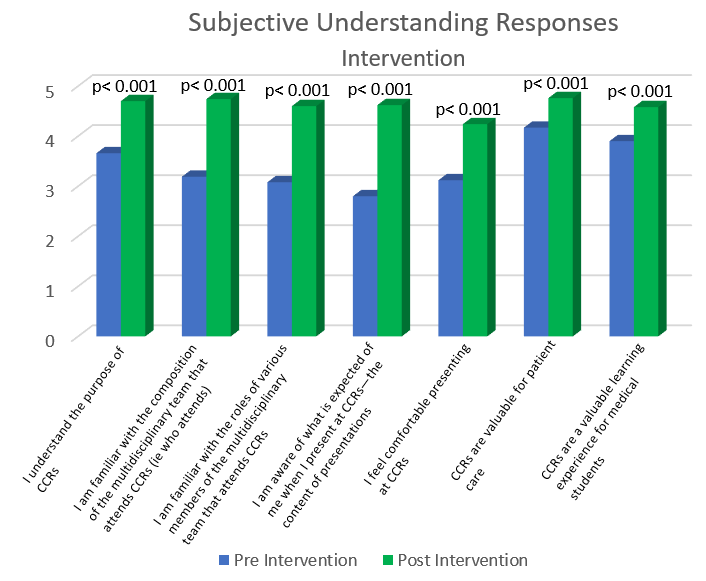
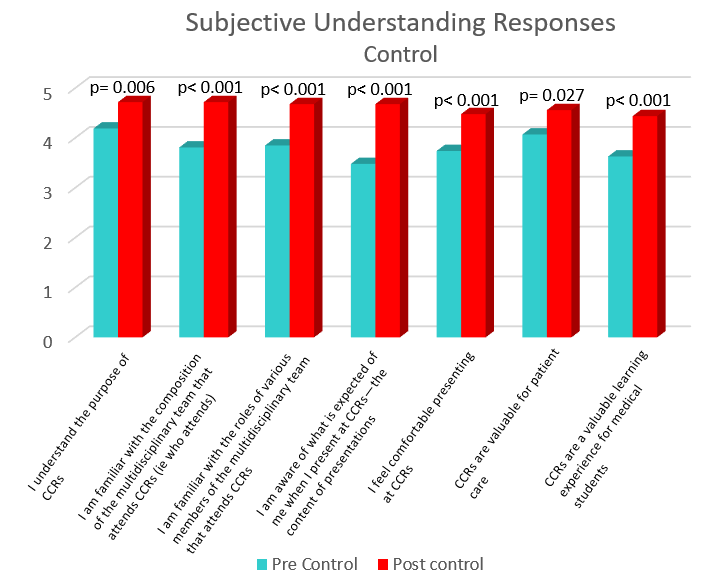
Results: Following the curriculum, medical students showed a statistically significant improvement in their subjective understanding of CCRs, including the purpose, the participants, and the expected content of CCRs (p<0.001) (see attached graphs). There was a trend towards significance between the intervention and control groups on charge nurse survey evaluations (p= 0.06), with the majority of responders reporting students were familiar with patients hospital admission reason, their potential discharge date, and barriers to discharge. The lack of statistical difference between groups likely had several causes, including low charge nurse survey response rate resulting in an under powered analysis, inter-student discussion during the month, and increased encouragement of team attendings and residents to coach students on CCR presentations prior to presenting.
Conclusions: Our study shows that with a brief curriculum, medical students become far more comfortable with the details of CCRs and feel more prepared to participate in them. This supports the addition of a CCR curriculum into third and fourth year medical student education.