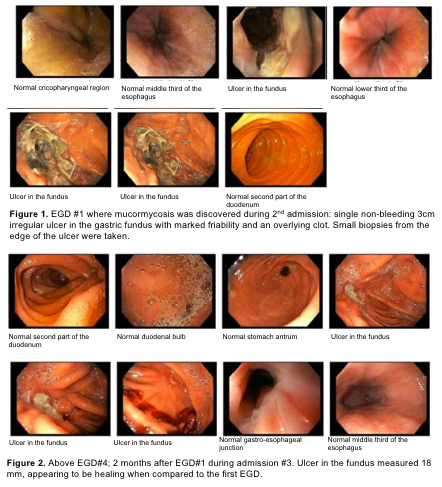
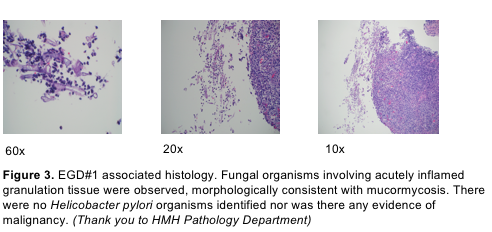
Case Presentation: A 32 year old male with alcohol abuse and Kratom use was initially hospitalized for 7 days for acute alcoholic pancreatitis and discharged with corticosteroids due to concern for alcoholic hepatitis. On day 14 of corticosteroids, he was readmitted for acute blood loss anemia requiring transfusion. Initial esophagogastroduodenoscopy (EGD) showed gastric mucormycosis on biopsy of a 3 cm gastric fundal ulcer. Screening for additional risk factors was unremarkable, including an A1c of 5.5%. He was started on Amphotericin B and a second EGD showed ulcer improvement. Outpatient, he tolerated Amphotericin B well with minimal complications. Two weeks later, a third EGD was done outpatient with continued ulcer improvement. Following a 4-week course of Amphotericin B, he was transitioned to Posaconazole for maintenance therapy. During admission #3 for alcoholic pancreatitis, a fourth EGD showed further resolution of his ulcer. He was subsequently discharged with a three-month course of posaconazole.
Discussion: While rhinocerebral and pulmonary mucormycosis are more common, angioinvasive GI disease can also occur. Risk factors include diabetes (especially DKA), immunosuppression, and alcohol abuse. Risk factors associated with this case include recurrent alcohol abuse as well as recent corticosteroid use for suspected alcoholic hepatitis plausibly contributing to an immunosuppressed state. Kratom use could also be considered an exposure risk factor although studies are limited in this regard. This case report is unique in that a patient was successfully treated solely with anti-fungal therapy, which is unconventional as surgical intervention is usually required in the setting of failed traditional medical therapy
Conclusions: Although largely uncommon, this case illustrates how the culmination of known risk factors can often create the perfect environment for pathology. Interestingly enough, the patient’s concurrent suspected alcoholic hepatitis and subsequent corticosteroid administration shines light on plausible pathophysiological insight as to the nature of angioinvasive gastrointestinal mucormycosis. Furthermore, the patient’s use of a largely understudied substance (Kratom) exposes yet another likely agent and possible risk factor for disease in the setting of increasingly popular use of herbal supplements. Thankfully, use of a contextually unconventional treatment plan proved to be successful and opens the door for additional study into alternative non-surgical regimens for the management of gastrointestinal invasive mucormycosis.