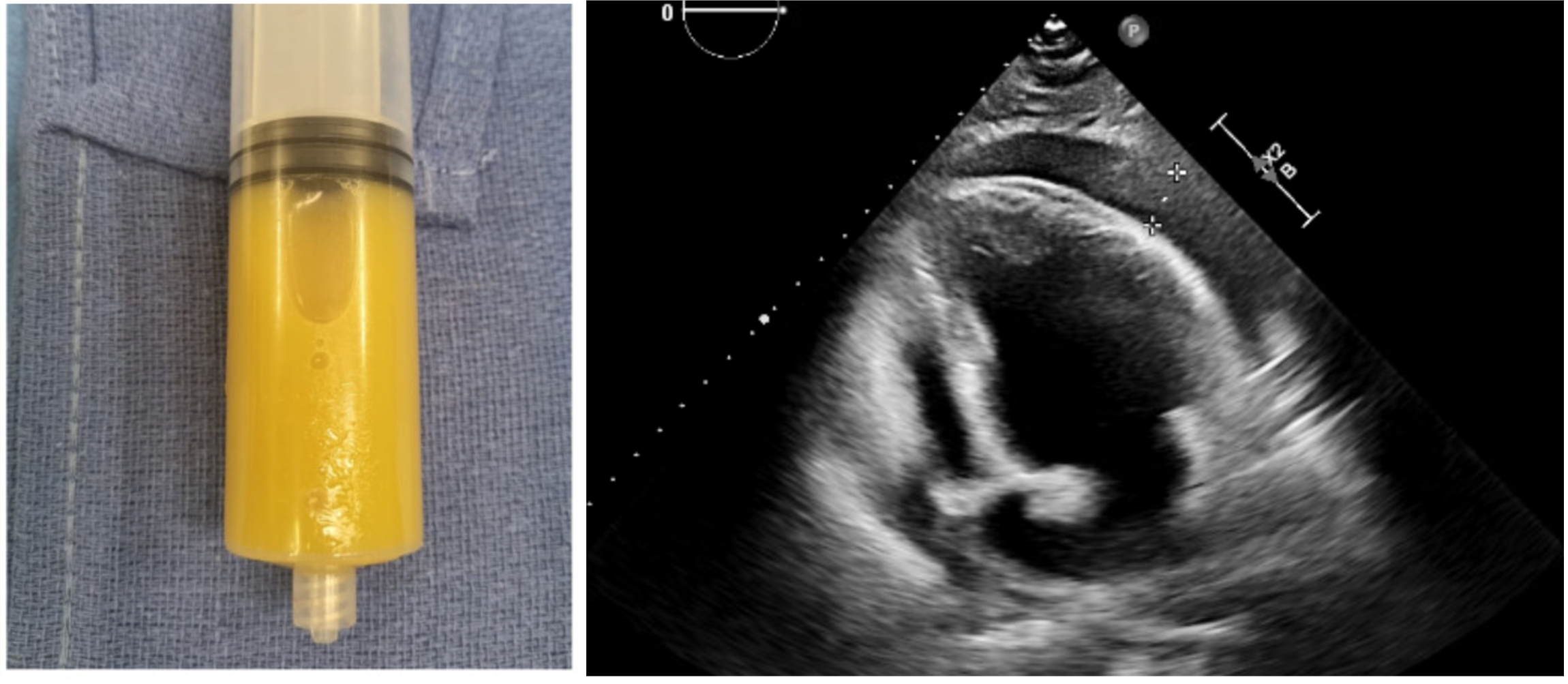
Case Presentation: Neisseria meningitidis, a gram-negative diplococcus, is widely known for causing meningitis and septicemia. However, its potential to trigger rare cardiac manifestations, such as pericarditis, often goes unrecognized. These atypical presentations can mimic common cardiovascular emergencies like myocardial infarction or pulmonary embolism, creating significant diagnostic challenges.A 44-year-old male with a history of type 2 diabetes, hypertension, obesity, and smoking presented with acute, severe pleuritic chest pain radiating to the neck and shoulders. Initial suspicion of acute coronary syndrome, based on subtle ST-segment elevation on electrocardiogram (EKG), was ruled out after coronary angiography showed no significant disease. Persistent symptoms prompted further evaluation, revealing a subsegmental pulmonary embolism (PE). Despite anticoagulation, the patient deteriorated, requiring intra-aortic balloon pump support. Laboratory findings, including leukocytosis and elevated procalcitonin, pointed toward a severe infectious process.Blood cultures confirmed Neisseria meningitidis, prompting immediate intravenous ceftriaxone. On day three, the patient developed pericardial tamponade with sinus tachycardia and pulsus paradoxus. Echocardiography confirmed a large pericardial effusion, and pericardiocentesis drained 260 mL of purulent fluid, which tested positive for Neisseria meningitidis. Persistent pericardial inflammation identified on PET scan led to the addition of colchicine for inflammation management.
Discussion: This case highlights the diagnostic and therapeutic complexities of managing meningococcal bacteremia with acute pericarditis, a presentation rarely documented in the literature. The overlap with more common cardiovascular conditions such as myocardial infarction or pulmonary embolism delayed recognition of the infectious etiology, emphasizing the need for a high index of suspicion in atypical cases. The subsequent development of pericardial tamponade and nonspecific aortic inflammation further complicated the diagnostic process, requiring advanced imaging modalities and a multidisciplinary approach to rule out autoimmune or vasculitic conditions.Therapeutically, intravenous ceftriaxone was pivotal in treating the bacteremia, but managing persistent pericardial inflammation required the adjunctive use of colchicine. While colchicine is well-established for idiopathic or autoimmune pericarditis, its role in infectious cases is not supported by robust evidence, reflecting a gap in the current literature. This case underscores the challenge clinicians face in balancing standard protocols with individualized care when established guidelines are lacking.The patient’s favorable outcome reinforces the importance of early recognition, microbiological confirmation, and multidisciplinary collaboration in managing rare and life-threatening cases. Advanced imaging played a crucial role in guiding management, particularly in distinguishing between infectious and autoimmune etiologies. The use of colchicine in this context warrants further investigation to define its potential benefits in similar cases.
Conclusions: The lack of guidelines for managing meningococcal pericarditis highlights the need to share knowledge of such rare cases. Increased awareness and research are essential to guide treatment and improve outcomes.