Background: Mentorship can help accelerate career advancement and professional development for pediatric hospitalists; thus, many Pediatric Hospital Medicine (PHM) divisions are creating formal mentorship programs. However, it is not currently known how many PHM divisions have mentorship programs or what aspects of mentorship are needed for hospitalists. Our study aimed to understand the current landscape of mentorship programs, as well as the desired domains, outcomes and types of mentorship needed in PHM.
Methods: Following content validation and piloting, we conducted a cross-sectional survey of listserv members of the American Academy of Pediatrics Section on Hospital Medicine Subcommittee of Division Directors. The 20-item electronic survey was administered anonymously from August-October 2020 to assess the characteristics of current mentorship programs, understand the needs of divisions without a mentorship program, and identify facilitators and barriers to program implementation and success.
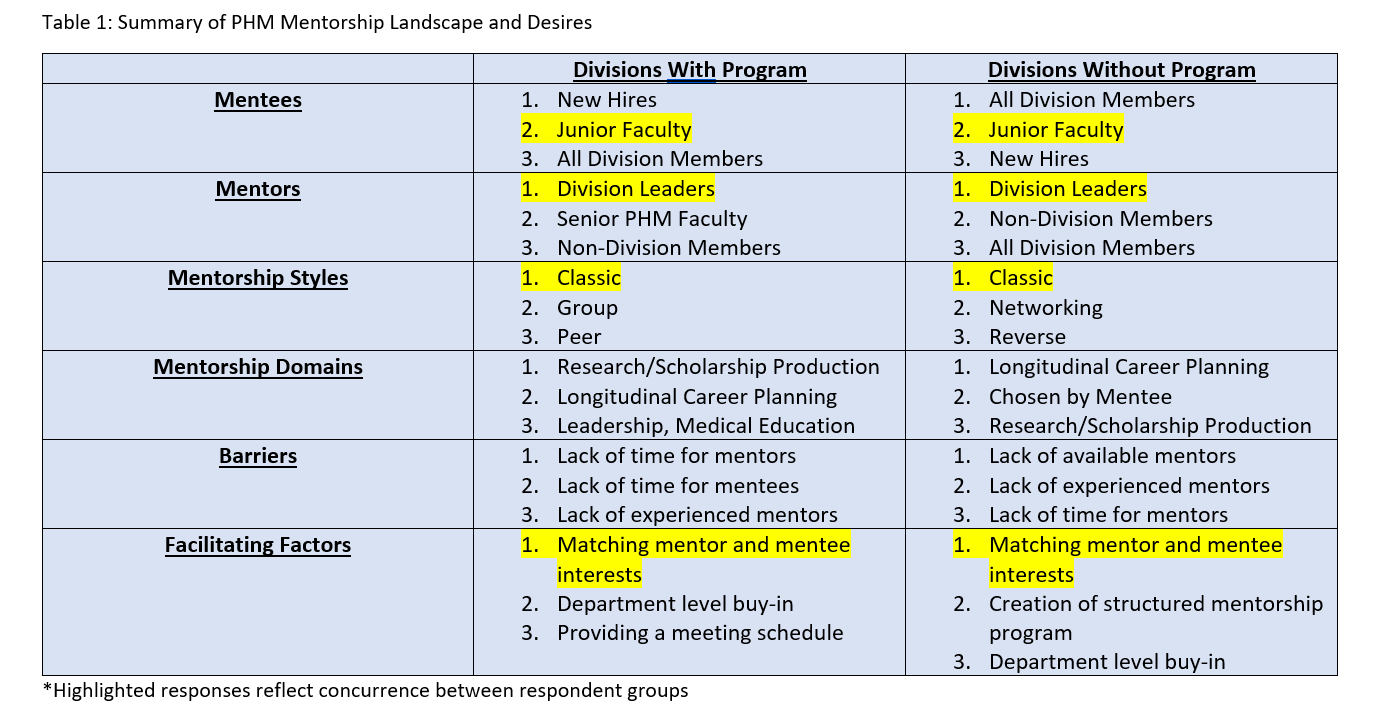
Results: A total of 64 out of 317 listserv members responded to the survey. Division directors mostly represented university-affiliated hospitals, with 10% of respondents from community hospitals. Most (76%) divisions had at least 25% of their faculty with less than 5 years’ experience and most (69%) had less than 20% of faculty at the associate professor level or above. Overall, 67% of divisions did not have a mentorship program in place. Of divisions with a mentorship program, 50% of mentees were early career hospitalists (new hires and less than 5 years’ experience), while 58% percent of divisions without a program would include all division members as mentees. Mentors outside the PHM division were utilized by 50% of current mentorship programs and desired by 42% of divisions without a program. While the classic mentorship style was most commonly used (79%) and desired (61%), more innovative styles such as networking (37%) and reverse mentorship (21%) were also identified. Directors preferred mentorship domains be chosen by the mentee, with longitudinal career planning identified as a priority. The most common facilitating factors for successful mentorship in PHM were matching mentor/mentee expectations and creating a formal mentorship program. The most common barriers were lack of time for mentors, and lack of experienced mentors in PHM (Table 1).
Conclusions: Most PHM divisions do not currently have a mentorship program for hospitalists. While divisions with mentorship programs primarily include junior faculty as mentees and utilize a classic mentorship style, those lacking a program are interested in creating a structured mentorship program individualized to the mentee that utilizes innovative mentorship styles. Opportunities for better mentorship in PHM include creating structured mentorship programs that match mentees and mentors based on shared interests, maximize access to senior PHM faculty and experts outside the division and allow mentees to determine mentorship domains.