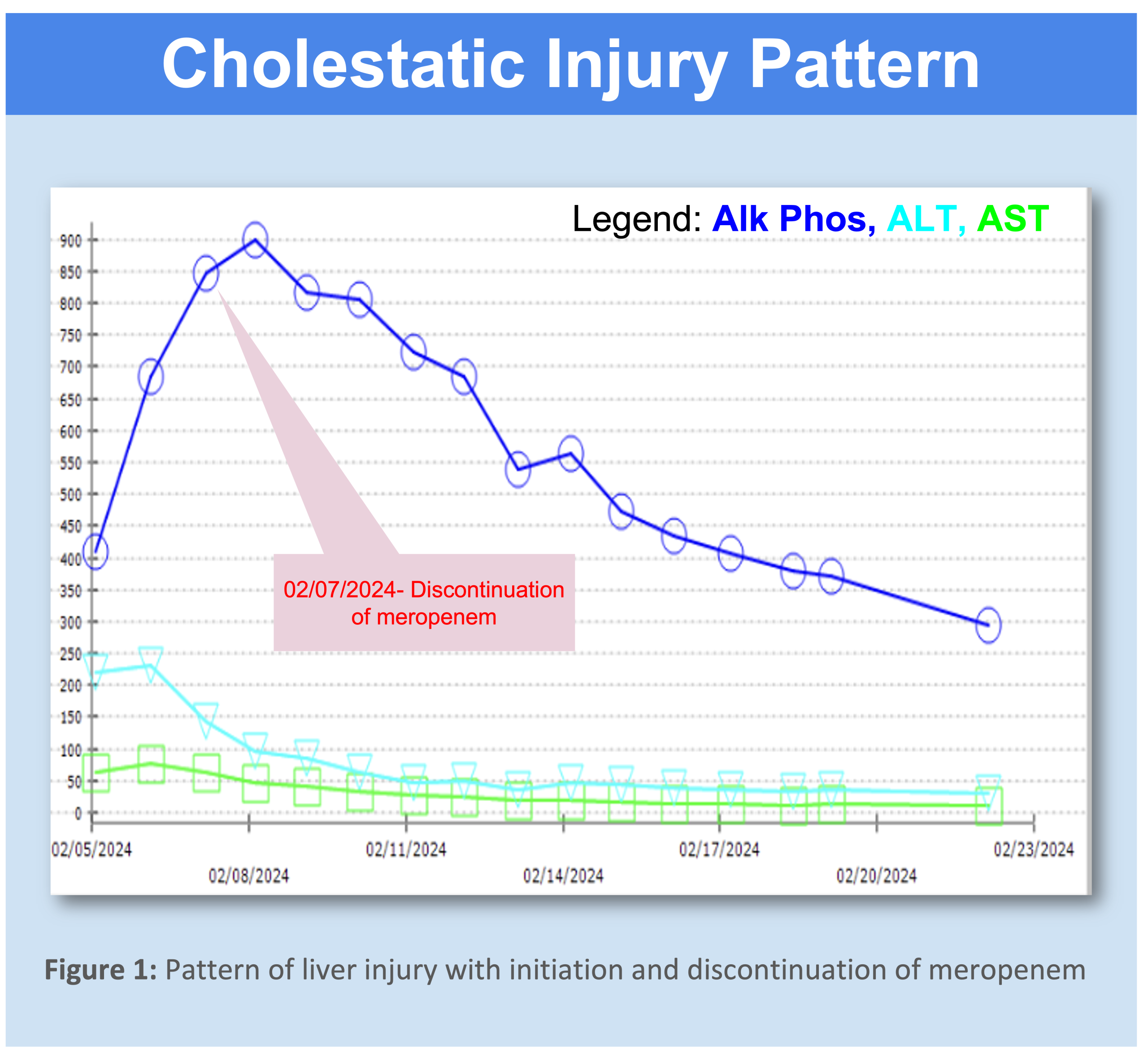
Case Presentation: We present a case of symptomatic meropenem induced cholestasis in a 57 year old male with insulin dependent diabetes complicated by polymicrobial foot ulcers that required multiple toe amputations. He presented with chief complaints of fatigue, decreased appetite, and weight loss. He was septic on arrival and was found to have wet gangrene on his left great toe. He was started on broad spectrum antimicrobials including meropenem, daptomycin, and micafungin given the polymicrobial nature of his osteomyelitis. One month prior to this admission, his serum aminotransferases were within normal limits and alkaline phosphatase was elevated at 345. During his hospital course, alkaline phosphatase, alanine transaminase (ALT), and aspartate aminotransferase (AST) levels all increased daily, with alkaline phosphatase being significantly higher than the other two. Additionally, the patient complained of persistent pruritus throughout the treatment period. On day 5 of treatment, alkaline phosphatase was 848, ALT was 64, and AST was 143. Bilirubin was also elevated at 1.7. The pattern of liver injury was suggestive of drug-induced cholestasis. The R value, used to determine the pattern of liver injury, was calculated at 0.15, highly indicative of a cholestatic injury (2). Gamma-glutamyl transferase levels were significantly elevated at 687, suggesting a hepato-biliary etiology for the alkaline phosphatase elevation. Other more common causes of cholestasis such as primary biliary cholangitis and primary sclerosing cholangitis were ruled out with right upper quadrant ultrasound and a negative evaluation for antimitochondrial and anti-smooth muscle antibodies. As such, meropenem was discontinued and levofloxacin and bactrim were started. The patient’s liver enzymes trended down after meropenem was stopped. Bilirubin immediately normalized after stopping meropenem. Pruritus resolved as well. Over the course of 2 weeks, the ALT and AST levels normalized. Alkaline phosphatase decreased to 294 after having peaked at 899. Due to the resolution of liver enzymes after discontinuing meropenem, we associate the cholestatic liver injury with meropenem use.
Discussion: Due to the resolution of liver enzymes after discontinuing meropenem, we associate the cholestatic liver injury with meropenem use. Cholestatic hepatitis attributed to the carbapenems is likely immunoallergic in nature and resembles the rare clinically apparent liver injury that has been linked to penicillins and cephalosporins. Vanishing bile duct syndrome is extremely rare but has been linked to antibiotic use. Liver biopsy is needed for definitive diagnosis; patients presents with progressive loss, destruction, and disappearance of the intra-hepatic bile ducts, leading to cholestasis.
Conclusions: Drug-induced liver injury (DILI) should be on the differential when a patient presents with abnormal liver enzymes and jaundice. Though meropenem is usually well tolerated, serum aminotransferase elevations have been reported in 1% to 6% of patients who are on meropenem for about two weeks. Although rare, meropenem-induced cholestasis has been reported to cause vanishing bile duct syndrome and cholestatic hepatitis. Mechanism of injury is not fully understood but may be due to immunoallergic reaction causing hepatotoxicity. This case serves to remind us that meropenem-induced cholestasis should be considered as a potential complication of a typically well tolerated antibiotic.