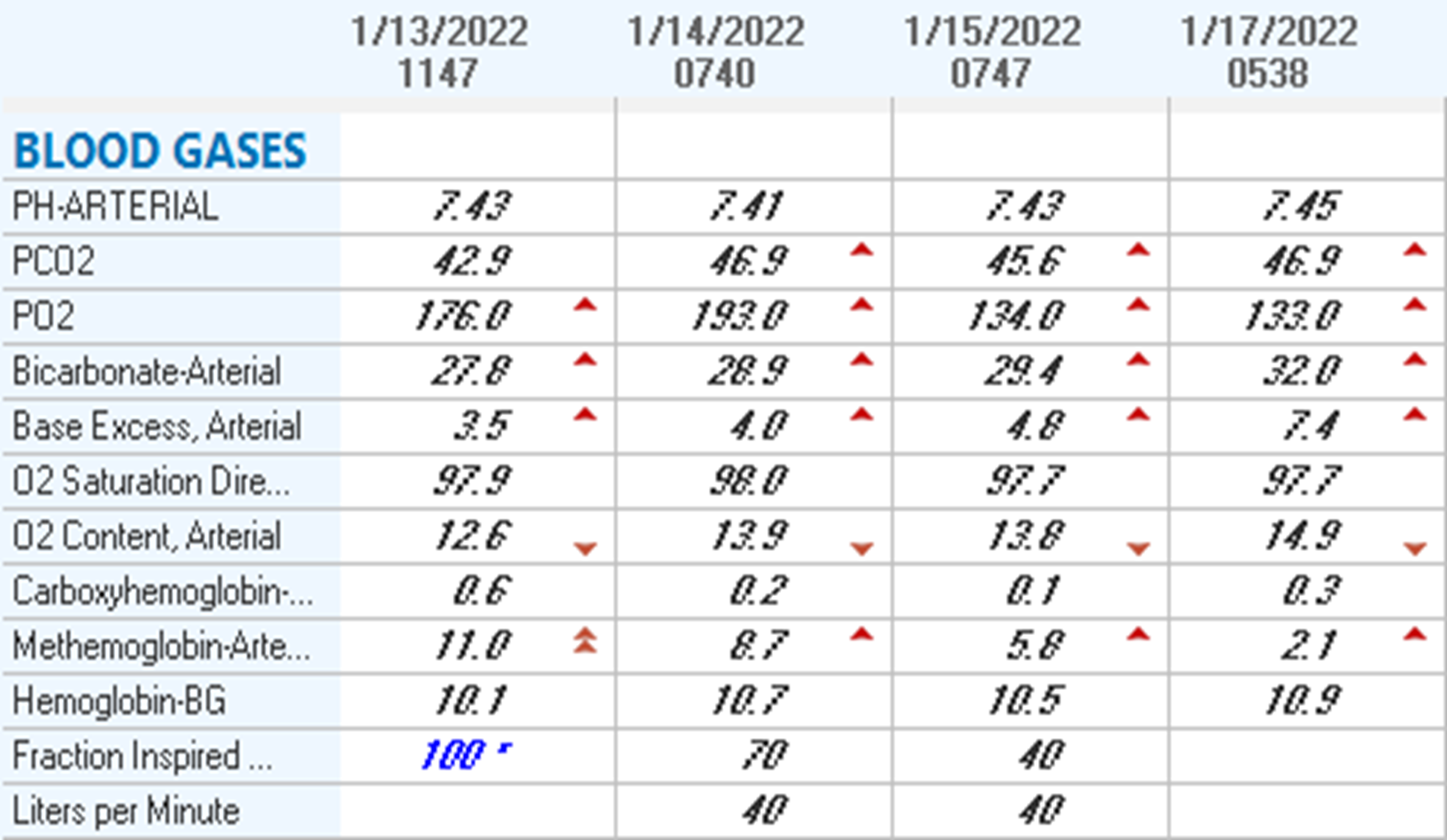
Case Presentation: A 69-year-old woman with ALL on chemotherapy and prior venous thromboembolisms being treated with rivaroxaban was admitted for symptomatic COVID19. She was dyspneic with pulse oximetry saturations in the 90s, so she was started on oxygen via nasal cannula, dexamethasone, and remdesivir. Initial chest X-ray, troponins, D-dimer, and BNP were unremarkable. Chemotherapy was held, though dapsone and valacyclovir prophylaxes were continued. Blood cultures grew gram positive organisms, so empiric broad spectrum antibiotics were initiated. On day three of admission, her hypoxia acutely worsened, and she eventually required high flow nasal cannula. Her arterial blood gas (ABG) on nonrebreather showed a pO2 well above 100 mmHg, a normal pH and pCO2, and a methemoglobin content of 11%. Repeat chest X-ray showed a developing pneumonia. Dapsone was discontinued, she was gradually weaned off supplemental oxygen to room air, and methemoglobin percentages improved on serial ABGs. Repeat blood cultures were negative. She was discharged one week after admission to outpatient hematology follow-up.
Discussion: Pulse oximetry detects hypoxemia by estimating arterial oxygen tension, but it can be inaccurate with hypoperfusion, hypothermia, hemoglobinopathies, and the presence of carboxy- or methemoglobin. Furthermore, these readings guide management and discharge of COVID inpatients, and inaccurate readings could cause delayed treatment of severely ill patients. Methemoglobinemia occurs due to the oxidation of iron in hemoglobin, making it incapable of carrying oxygen. Dapsone is a well-known cause, which can produce a low-grade methemoglobinemia as well as a more severe form with symptoms including cyanosis, headaches, arrhythmias, seizures, and death. Our case represents an interesting confluence of factors leading to hypoxemia: she had COVID19, a developing pneumonia, and a low-grade methemoglobinemia likely from prior to admission. She also had mild anemia with hemoglobins between 10-11 g/dL. Cardiac causes of hypoxemia were excluded with negative troponins, D-dimer, and BNP. Of note, methemoglobin tends to create falsely decreased readings on pulse oximetry, and at rising concentrations saturation may plateau around 85%. However, in this patient, we suspect its presence combined with infectious and hematologic causes of hypoxemia led to her clinical decline and increased level of care.
Conclusions: Hypoxemia can be life-threatening. It is typically attributable to respiratory or circulatory factors, such as limited diffusion or ventilation, shunting, and mismatching ventilation and perfusion from infection or pulmonary edema. These factors should be considered when working up hypoxemia. However, if present treatments are not helping, or if there are any doubts or inconsistencies in readings, further investigation of less common causes such as anemias or hemoglobinopathies is warranted. This is especially important for complex, hypoxemic patients with multiple comorbidities or polypharmacy, as they may have multifactorial causes of their presentation.