Background: For peripherally compatible infusates planned for <14 days duration, existing appropriateness criteria and guidelines recommend midline catheters instead of peripherally inserted central catheters (PICCs). However, there is wide variability in clinical practice and outcomes associated with midline devices. We describe our three-year experience with midline catheters at a large Veterans Administration tertiary-care medical center.
Methods: In June 2016, our trained vascular access nurses started placing midline catheters (PowerWand 10 cm, Access Scientific (R)) according to criteria established by the Michigan Appropriateness Guide for Intravenous Catheters (MAGIC). Midline insertions were performed under ultrasound guidance, using sterile technique, and with maximal sterile barrier precautions. We retrospectively collected demographic and clinical data from the medical record of every patient that received a midline catheter from June 2016 until May 2019. The occurrence of catheter-related complications, including major (e.g. venous thromboembolism or catheter-associated bloodstream infection) or minor (e.g. catheter occlusion, migration, kinking, infiltration) events were assessed up to 70 days after insertion.
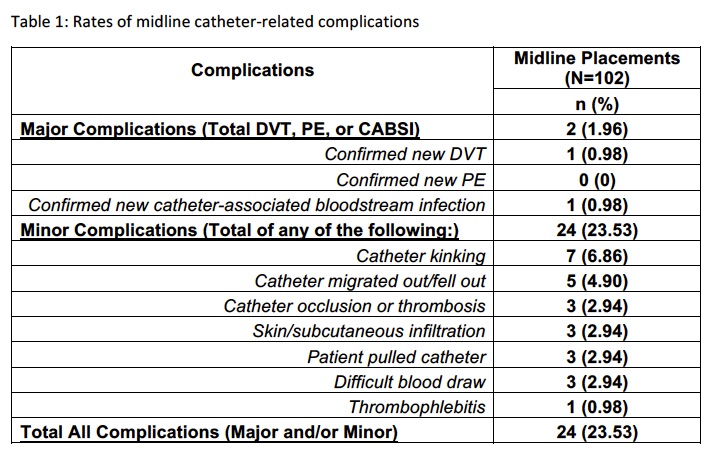
Results: Of the 102 patients that had a midline placed during the study period, 55 (53.9%) were for antibiotic infusion and 43 (42.2%) for difficult access. A total of 73 (71.6%) midlines were placed in the general inpatient ward, 11 (10.8%) in the intensive care unit and 18 (17.7%) in a post-acute care setting. The midline catheters lasted through the completion of therapy in 77 patients (75.5%). Of the 84 midlines that were placed during hospitalization, 32 (31.4%) were removed prior to discharge and 32 (31.4%) were removed after discharge owing to therapy completion. The median dwell time of all devices was 12 days (interquartile range, 6 to 21 days). Catheter-related complications occurred in 24 patients (23.5%), including catheter kinking (7 patients, 6.9%), catheter migration (5 patients, 4.9%), and catheter occlusion (3 patients, 2.9%). Only 2 patients experienced major complications with midlines: one deep vein thrombosis (1%) and one catheter-associated bloodstream infection (1%).
Conclusions: Midline catheters appear to be effective and safe for short-term vascular access in patients requiring peripherally compatible infusates. While the rate of major complication is low, minor complications that necessitate device removal are common.