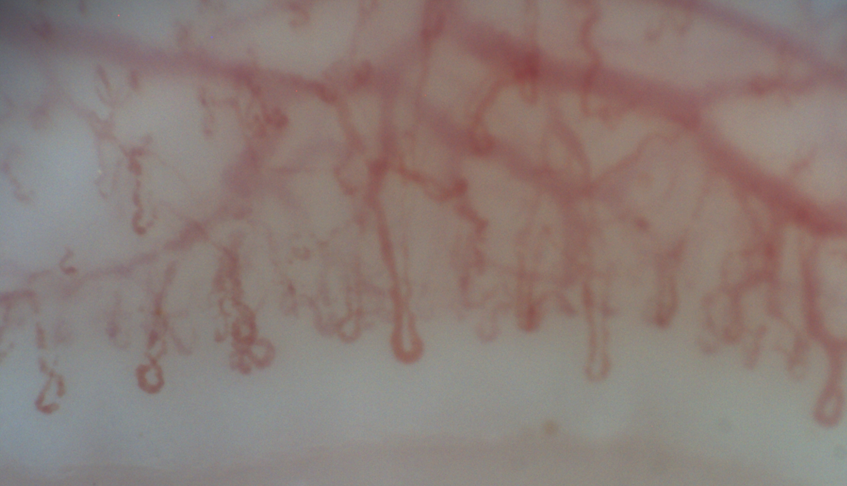
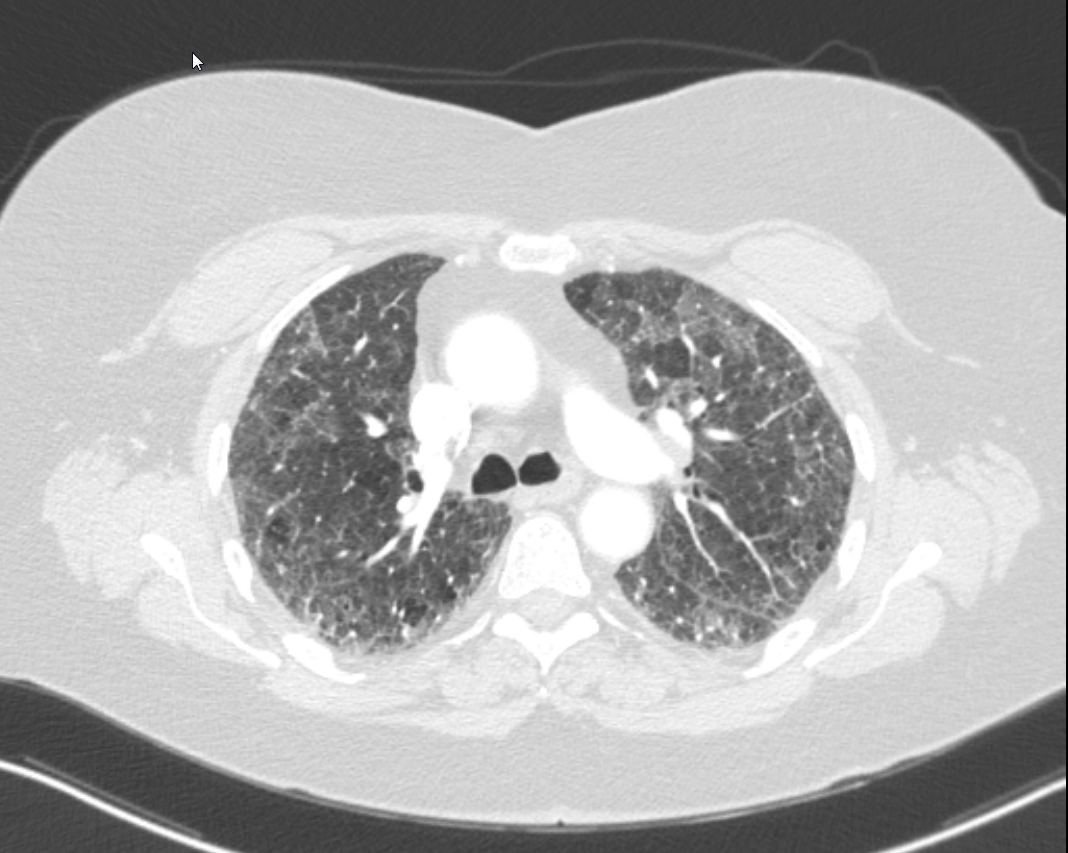
Case Presentation: 64-year-old female is admitted for workup and management of subacute, progressive dyspnea, pleuritic chest pain, dry cough, and new oxygen requirement. History is significant for plaque psoriasis on adalimumab (initiated 3 months prior to presentation), ulcerative colitis status post proctocolectomy, sicca symptoms, Raynaud’s phenomenon, GERD, maternal history of rheumatoid arthritis, and a 50-pack-year smoking history. CT showed moderate, multifocal GGOs consistent with nonspecific interstitial pneumonia (NSIP) or usual interstitial pneumonia (UIP) without honeycombing. Pulmonary function testing showed severely reduced DLCO. Ejection fraction was 60% without significant echocardiographic abnormalities. Labs remarkable for normal leukocyte count; moderately elevated ESR and CRP; and mildly elevated RNP, LDH, and aldolase. Rheumatologic and infectious testing (including bronchoalveolar lavage) was otherwise negative. Transbronchial biopsy showed bronchiolar wall and parenchyma without neoplasm or granuloma. Video capillaroscopy confirmed secondary Raynaud’s. Adalimumab was stopped, and she was started on prednisone 30 mg daily. She improved clinically and was discharged with home oxygen and plans for outpatient rheumatology and pulmonology follow up. Repeat CT chest one month later showed significant improvement in GGOs but persistence of fibrotic ILD. Pulmonology believed the remaining disease represented UIP versus NSIP related to underlying connective tissue disease. Rheumatology felt that the ILD with elevated RNP in the setting of her other rheumatologic symptoms were suggestive of mixed connective tissue disease (MCTD). Azathioprine was started with plans to wean the prednisone. She has since been improving clinically.
Discussion: Tumor necrosis factor inhibitors, like adalimumab, have been implicated in rare cases of interstitial pneumonia with a prevalence of 0.5% to 3%. ILD occurs in > 50% of those with MCTD. Careful consideration should be given to the underlying cause as adalimumab-induced ILD is a diagnosis of exclusion after ruling out infectious and cardiac etiologies. It is important to recognize fibrotic lung disease independent of the GGOs from adalimumab, especially when ILD persists despite discontinuation of the offending agent. Removing the adalimumab is often sufficient, but corticosteroids can be utilized in more severe or refractory cases. Fibrotic changes in the setting of connective tissue disease may require prednisone or other steroid-sparing agents, like azathioprine.
Conclusions: Adalimumab is an uncommon cause of interstitial lung disease (ILD). Patients on adalimumab for connective tissue disease can have a mixed ILD with fibrotic changes in addition to the ground glass opacities (GGOs) resulting from adalimumab.