Background: The Institute for Healthcare Improvement’s Age-Friendly Health Systems (AFHS) initiative calls for providers to ensure that older adults move safely to maintain daily function. However, studies show that about a third of hospitalized older adults have bed rest orders, most of which are not medically indicated. Therefore, at our 537-bed community teaching hospital, we have developed and piloted the “Mobilizing Older Adults using BMAT, Interprofessional Leadership, and Education (MOBILE)” quality improvement intervention.
Purpose: The purpose of MOBILE is to ensure older adult patients increase mobility during their hospitalization by empowering bedside nurses (RN) with the knowledge and tools to perform early and timely mobility assessments that guide physician activity orders and RN care plans.
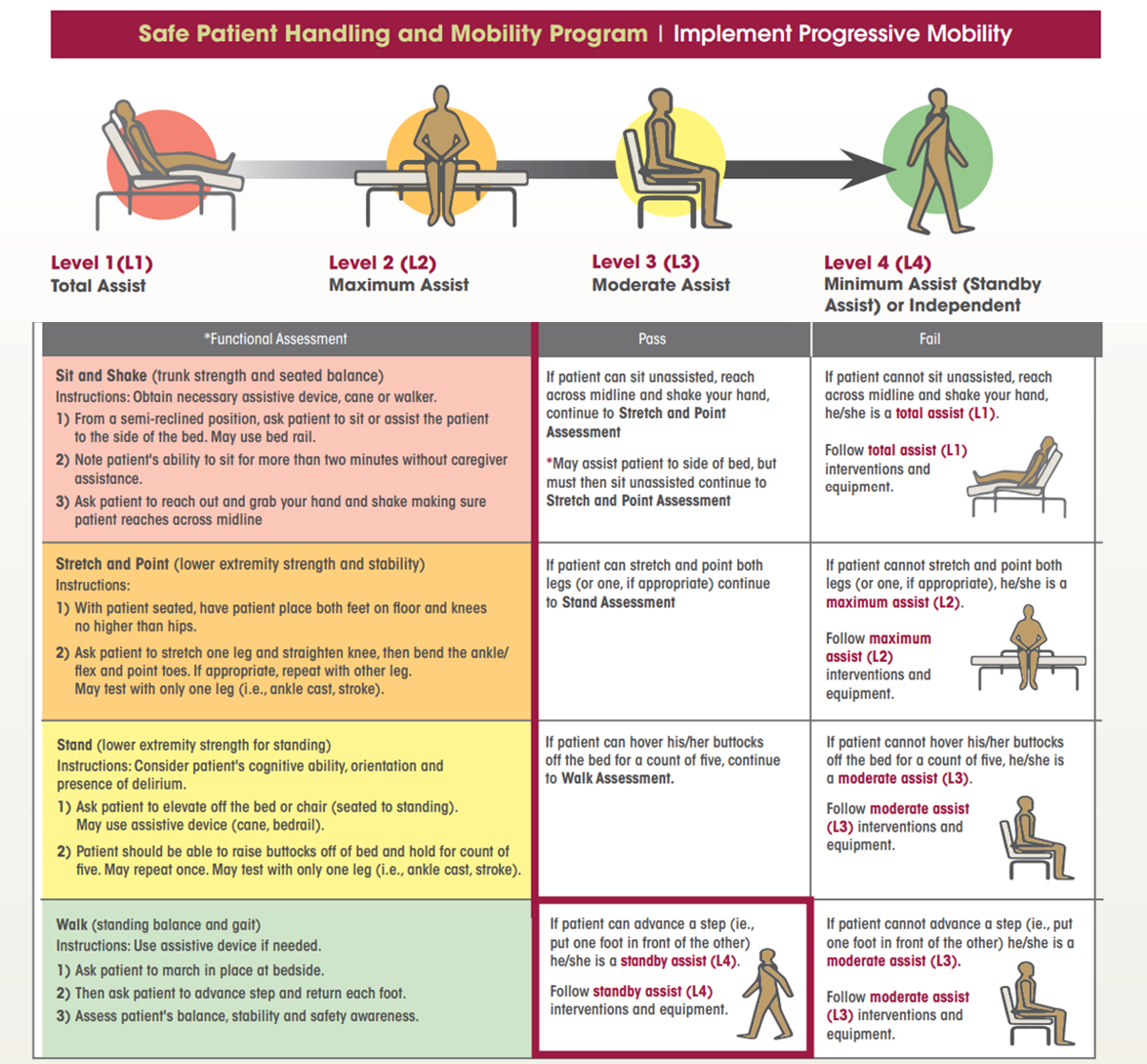
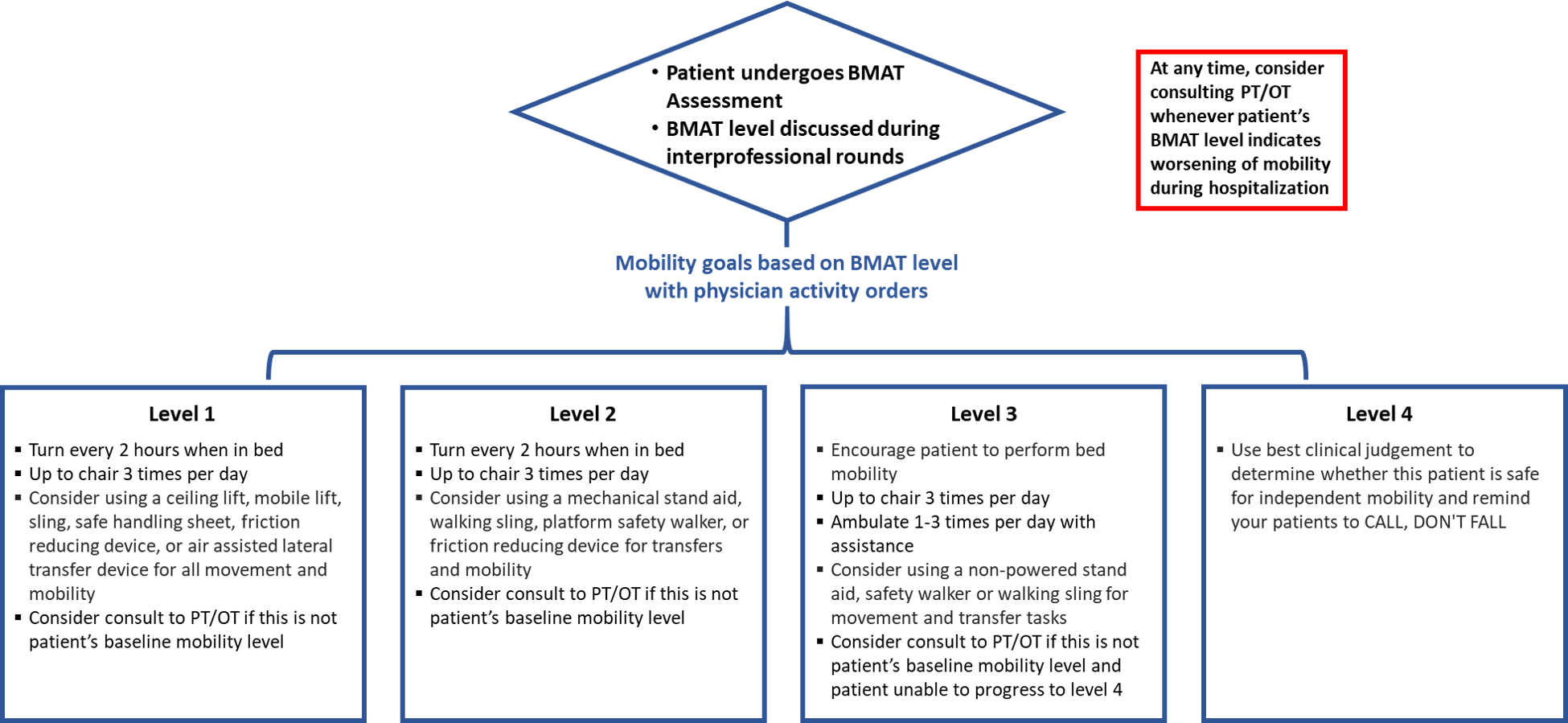
Description: In October 2022, we piloted MOBILE at our 13-bed Acute Care for Elders unit. We started with in-service training for RNs on the importance of mobility in hospitalized older adults as part of the 4Ms framework (What Matters, Medication, Mentation and Mobility) of an AFHS. We surveyed RNs on their knowledge around the importance of inpatient mobility and perceived barriers to mobilizing patients. RNs recognized the need to mobilize patients but described lack of understanding of patient’s current mobility status, time and staffing constraints, and potential falls as barriers. We then conducted one-on-one training on the Bedside Mobility Assessment Tool (BMAT), a validated tool designed for use by bedside RNs. BMAT requires patients to perform 2 minutes of functional tasks, which results in a mobility level from 1 to 4 (Fig. 1). It is performed on admission, on every shift, and when a significant clinical change occurs. The assessed mobility level is then shared at interprofessional rounds, where a tailored inpatient mobility plan is created, and corresponding physician activity orders are placed. For patients below their baseline mobility, consults are placed to physical and occupational (PT/OT) therapy (Fig. 2). We assessed MOBILE intervention performance in December 2022, which included 84 patients ≥65 years admitted to the unit. After excluding patients who expired or admitted to hospice, 43 (54%) of the 80 eligible admissions had BMAT completed at least once during hospitalization with 11 (26%) assessed upon admission. The most common BMAT level was level 3 (54%), followed by level 4 (28%), and levels 1 and 2 (9% each). The shift-to-shift compliance with BMAT was 16%. Utilization of BMAT was hindered by the electronic medical record (EMR) in that this intervention was not integrated within the standard RN care shift documentation, thus requiring them to use a separate flowsheet to record their assessment. BMAT compliance was also lower when float RNs were covering the unit. RNs reported that BMAT gave them the confidence to ensure early patient mobility, by keeping both the patient and staff safe from injury.
Conclusions: The interactive education and one-on-one BMAT training were integral to the success of MOBILE. Barriers to success included suboptimal EMR organization, competing clinical demands and staff turnover. We are collecting data to evaluate the impact of MOBILE on hospital length of stay, hospital-acquired pressure injuries and falls, PT/OT consult rate, and post-acute care utilization. Future plans include evaluations to assess the facilitators and barriers in adoption, fidelity and sustainability of MOBILE with a priority of improving shift-to-shift BMAT assessment compliance rate.